Social Care Sector COVID-19 Support Taskforce: final report, advice and recommendations
Updated 12 October 2020
Applies to England
Executive summary
The COVID-19 (coronavirus) pandemic of 2020 has presented an unprecedented challenge for social care. The response has not been without significant challenges at all levels of the sector. Every day we have learned more about the virus and have adapted accordingly. In a year where we have mourned the tragic deaths of every person due to this virus, we have also seen the remarkable efforts of individuals, teams and organisations, working together to try to provide the safest care of the highest quality possible.
There have been many examples of innovative best practice which have emerged during the pandemic, of which several case studies are included in this report, and we have heard the stories of the most dedicated and inspirational care being provided by care workers and colleagues. In a year where society has shown its value and high regard for key workers, this report sets out how we can best support all our social care colleagues as the pandemic response moves towards the autumn and into winter.
The Social Care Sector COVID-19 Support Taskforce was commissioned in June 2020, with this report seeing the completion of its work in August 2020. The taskforce was set up to oversee the delivery of 2 packages of support that the government had put in place for the care sector: the Social Care Action Plan and the Care Home Support Plan. In addition, the taskforce was asked to support the government's work on community outbreaks – areas of the country that needed particular help and intervention to deal with higher rates of infection – and advising and supporting local places to consider and respond to reducing the risk of infection in care homes and the wider social care sector. Its further remit was to provide advice on the requirements for the response to COVID-19 in the next few months, ahead of and into winter.
The taskforce has been led by David Pearson, former President of the Association of Directors of Adult Social Services (ADASS), reporting to the Minister of State for Care. Taskforce membership consisted of leaders from across government and every part of the social care sector. Eight advisory groups were established to explore specific areas of care, namely:
-
black, Asian and minority ethnic (BAME) communities
-
carers
-
good practice, guidance and innovation
-
mental health and wellbeing
-
older people and people living with dementia
-
people with learning disabilities and autistic people
-
self-directed support
-
workforce
The organisations and their leaders involved in the taskforce all responded to urgent requests for information, and provided expert views and analysis in support of the taskforce objectives on particular pieces of work and evidence. This includes the chairs and participants of the advisory groups who convened at short notice to provide evidence and exceptional advice and insight.
The taskforce carefully considered an extensive range of issues in relation to the social care sector as a whole, brought together as key themes. These included the provision of personal protective equipment, COVID-19 testing arrangements, the winter flu vaccination programme, infection prevention and control, and issues of funding. The taskforce examined a number of issues relating to the workforce and family carers (unpaid), including how best to restrict the movement of people between care and health settings. Among other themes, the taskforce reviewed the role of clinical support within the sector, the availability and application of insights from data, and implications of inspection and regulation.
As a result of the dedicated and diligent work of all members of the taskforce and advisory groups, this report is now able to set out the action that will need be taken to reduce the risk of transmission of COVID-19 in the sector, both for those who rely on care and support, and the social care workforce. This report sets out how we can enable people to live as safely as possible while maintaining contacts and activity that enhance the health and wellbeing of service users and family carers.
Throughout this report, a number of recommendations are made based on learning from the first phase of the pandemic. They range from 'quick wins' to consideration of topics that will require a degree of more substantial change and/or additional resource. In addition, there are a number of supporting recommendations in the annexed reports of the subject-specific advisory groups, which should be considered in tandem with the main report recommendations.
As we move towards winter and a potential second phase of the pandemic, this report has established the requirements to increase resilience in the sector. It sets out 3 key elements – the national offer, the regional response and the local response. The Department of Health and Social Care (DHSC) intends to publish a winter plan for adult social care. Following its publication, one recommendation is that each local authority and care provider should have in place its own winter plan to build resilience and give confidence to the public. Along with other measures that the country will need to continue to take as it responds to the coronavirus threat, all of the recommendations in this report should help improve resilience in the social care sector and help save lives this winter.
Foreword
A test of any country is the degree to which it supports and enables those who need care and support to stay safe and to lead the best lives they can. The government established the taskforce at a time of the most unprecedented attack on the health and economic wellbeing of the country and large parts of the world. The ambition, as set out by the Secretary of State is, as far as possible, to keep people safe and reduce the risks of the COVID-19 virus, while maintaining their wellbeing.
The challenge is significant. The measures require investment by government and policy initiatives rapidly translated into action in the 38,200 settings in which people in this country receive their care and support. Responding to this challenge, for the rest of the pandemic will require a collective leadership effort from the government and all parts of a diverse sector and other public services including the NHS, acting together as one. The taskforce was encouraged, by the government, to be ambitious and bold. The report, advice and recommendations are therefore wide-ranging.
The taskforce consists of leaders from across government and from the sector, representing many of the very organisations and specialisms that are an essential part of the make-up of any social care sector. People working on a daily basis with the taskforce have been drawn from across every part of the sector. The organisations and their leaders have responded to urgent requests for information, views and analysis in support of the objectives of the taskforce on particular pieces of work and evidence. This includes the chairs and participants of the advisory groups who have convened at short notice to provide evidence and advice on what is needed for the coming months and for the duration of this pandemic. I am very grateful for the level of goodwill and assistance that has been offered to the taskforce and its ambition. It has built upon the work that had taken place on the Social Care Action Plan and the Care Homes Plan by DHSC.
Technical skill, equipment and technology are an essential part of a modern social care system, but the effectiveness of social care is determined largely by the people who work in it. We have all heard about the struggles of grappling with the virus, resources, the guidance and making the rapid adjustment to the way that services are delivered and new priorities.
We know more about the virus than we did at the beginning of the pandemic, gaining more knowledge every day. It is our collective responsibility to ensure that we use the experiences, knowledge and understanding gained so far this year to ensure that the sector is resilient in dealing with what lies ahead.
We have heard about the many extraordinary acts of kindness, commitment and determination to ensure that people's needs are met in very unusual and demanding circumstances by those working in social care. This will be required in large measure during the next phases.
David Pearson CBE, Chair – Social Care Sector COVID-19 Support Taskforce
Background
The social care sector in England is diverse in nature, with a workforce of 1.5 million in 18,500 organisations providing care and support in, or from, 38,000 settings. The sector involves public, not-for-profit and privately-run provision which is funded mainly either by the people who use the services or by 152 local authorities (those local authorities with adult social care responsibilities, known as 'upper tier'). NHS Clinical Commissioning Groups also fund or commission some social care as part of jointly funded Continuing Healthcare packages and in the context of current discharge arrangements. Social care is also funded privately by individuals, based on their assets and income. Approximately half of all people who receive social care fund themselves in care homes and an estimated 30% fund the care provided in their own homes. More than half of the social care budget is spent on people aged under-65. Although when people consider social care, care homes and home care spring to mind, there is a rich diversity of other provision, including 65,000 people who employ 145,000 personal assistants. There is also substantial provision of housing with support including the provision of technology-enabled care.
Social care provides a diverse range of services to meet needs. There are services that are focused on prevention, by reducing risk to people's physical or emotional wellbeing and promoting independence. Alongside the more traditional services of care homes and home care are a wide range of options, including approaching 240,000 people who receive a direct payment, with 75,000 of these employing their own staff. This is one component of "self-directed support" which affords the opportunity of enhancing people's choice and control over their lives. Wider networks of support include housing with support and technology enabled care.
COVID-19 is a pernicious virus that has led to premature deaths and had a major impact on the lives of everyone. From the first reported cases of the virus in China, in December 2019, its spread has been dramatic. While the scientific understanding of the virus continues to grow, we now know far more about the virus than we did at the beginning. It disproportionately attacks those who have long-term conditions or disabilities and is particularly dangerous in situations where intimate personal care needs to be provided.
In social care, the 3 main variables that influence the level of risk are the nature of the virus; the circumstances and health of those people at risk of being infected or already infected; and the settings in which they receive care and support. For example, the evidence points to higher levels of risk in large residential settings compared with people's own homes.
It is also the case that, as the BAME Communities Advisory Group point out in their report, various studies have evidenced the disproportionate impact of COVID-19 on BAME people and differences with other ethnic groups, including higher levels of mortality than the white population. As the report goes on to say, the reasons for this are likely to be multi-faceted, including relative deprivation. It is also the case that a greater proportion of the population were involved in key worker roles increasing the risk of exposure to infection. The report highlights the issues that were raised by the workforce, service users and carers they consulted and the need to ensure the engagement of BAME communities in better understanding the issues faced and the solutions. This has long been the case, but it has been reinforced by the experience of COVID-19 as an essential prerequisite of effectively addressing the needs and risks of BAME communities, including the concern of unjustified differential treatment. It is with this perspective and through this lens that social care policy makers, commissioners and providers need to consider every policy, action and service, including the contents of the rest of this report.
In responding to COVID-19 there is also a balance to be struck between reducing the risks of the virus and the need to receive care and support. As the Self-directed Support Advisory Group argue, there is the need to pay attention and assure ourselves that the human rights obligations are being considered and adhered to in all the circumstances. Balancing these important considerations is not only a legal requirement, but a way of helping to ensure that the interests of the people who use services is considered and addressed, taking into account all their needs and rights.
The more we know, the more we can target our actions to mitigate these risks. It has become clearer over recent months, through international research,[footnote 1] [footnote 2] that many people in care settings who have been infected with COVID-19 (typically over 50%) are either pre-symptomatic or asymptomatic and can transmit the virus. It is a disease that is often invisible, making it particularly dangerous.
It is not possible to eliminate the risk of infection where care and support is being provided. In areas of sustained community transmission, the risks of infection are very high. However, nothing is inevitable and all of us can help by protecting ourselves from infection and inadvertently transmitting the virus to people who provide or receive care. Despite the difficulties, there have been many examples of good practice and 62% of care homes have not experienced an outbreak.
In response to COVID-19, a taskforce for the social care sector was commissioned, beginning its work on 15 June 2020 and completing its work at the end of August 2020. At the time the government formed the taskforce, the Social Care Action Plan had been in place for 2 months and the Care Home Support Plan had been launched a month earlier. Much work had been undertaken by the government and the DHSC in the preparation and implementation of the Social Care Action Plan and the Care Home Support Plan and therefore progress on both these initiatives was underway among local government and providers.
The taskforce
Terms of reference
The letter from the Secretary of State, on 17 June 2020, set the remit of the taskforce to:
1) oversee the delivery of the Care Homes Support Plan with a view to ensuring that this is delivered and implemented by every care home in every local authority in England
2) oversee the delivery of the Adult Social Care Action Plan (published 15 April 2020)
3) provide clear advice on what needs to be in place across all parts of the care sector in England to respond to COVID-19 over the coming months, and ahead of winter
The government provided £3.7 billion general grant for local government, in 3 tranches, from March 2020 through to June 2020 – part of this was intended for social care. The government also made available £600 million to local authorities and providers as part of the announcement of the Care Homes Support Plan in May 2020.
Our scientific understanding of how the virus works and its impact on both people who use social care services and the social care workforce, in the different settings where people receive care and support, is rapidly evolving. A plan written today is likely to be out of date tomorrow.
In preparing for winter and beyond, the taskforce believes that the government needs a plan that will lead to greater capacity, capability and resilience, reducing risk through to spring 2021.
Understandably and rightly, there is a high level of focus on controlling infection. But as the Terms of Reference state, we must seek to enable people to live as safely as possible, while maintaining contacts and activity that enhance the wellbeing of service users, carers and families. It is very important that distancing people from the virus does not disconnect them from family, friends and other sources of support. Nor must it disconnect them from essential services, all of which help to maintain people's health and wellbeing and, ultimately, help to reduce premature mortality.
As the letter from the Secretary of State said:
This will ensure that concerted and determined action is taken to reduce the risk of transmission of COVID-19 in the sector, both for those who rely on care and support and the social care workforce. It will support the national campaign to end transmission in the community. This taskforce will also consider the impact of COVID-19 on the care sector over the next year and advise on a plan to support it through this period. It will seek to enable people to live as safely as possible whilst maintaining contacts and activity that enhance the health and wellbeing of service users and their family carers.
The emphasis, for the government and the sector, for the remainder of the pandemic, must be to explore and apply every of possible method to protect and connect.
The taskforce was established to maintain strong arrangements to keep under review any new national and international evidence on the impact of COVID-19 and advise on its application to the English social care system.
At the start of the taskforce, the government put in place arrangements for overseeing the response to local community outbreaks. The taskforce Chair was invited to join the Joint Biosecurity Centre (JBC) Local Action Committee (Gold). The taskforce then took on the role of linking with the sector on the social care implications of managing local community outbreaks and establishing arrangements that ensure an effective interface with NHS Test and Trace and the Contain function.
The taskforce has supported the implementation of key pre-existing government strategies and plans, and shaped and delivered new initiatives. This report will provide advice on what more could and should be done to support the sector and, most importantly, those who use services.
It is worth noting that the focus of the taskforce has been on social care and COVID-19, not the long-term reform or the sustainability of the system. As well as these areas, other elements of the social care system are covered in the general work of the DHSC and, in particular, the work on the Care Act 2014 duties and assessments are overseen by the chief social workers. Although a few authorities did apply Care Act easements, at the time of writing, no local authorities are applying these measures. However, during the course of our work, a number of organisations raised with us the concern that Care Act duties may be subject to prioritisation by local authorities. It is important that the government and local authorities keep this under review, including the degree to which all Care Act responsibilities are being delivered.
Also out of scope is the financial sustainability of the sector. However, the pandemic and the work of the taskforce has occurred in the context of universal recognition by the government and opposition parties of the need for investment and reform. In some instances, there is a fine distinction between the issues that have impacted upon the sector as a result of COVID-19 and pre-existing fragility and fragmentation. Both local authorities and providers have emphasised their concern about the wider financial sustainability of the system. The advisory groups did raise issues that were out of the direct scope of the taskforce but the chair undertook to ensure that these points were noted so that they could be considered in the context of the separate work that the government is undertaking on long-term reform.
Membership
Taskforce
-
David Pearson (Taskforce Chair)
-
James Bullion (President, Association of Directors of Adult Social Services)
-
Clenton Farquharson (Representative with lived experience of care services)
-
Dr Jeanelle de Gruchy (President, Association of Directors of Public Health)
-
Dr Jenny Harries (Deputy Chief Medical Officer for England)
-
Emily Holzhausen (Director of Policy and Public Affairs, Carers UK)
-
Dr Nikita Kanani (Medical Director of Primary Care, NHS England/Improvement)
-
Christina McAnea (Assistant General Secretary, Unison)
-
Sarah Pickup (Deputy Chief Executive, Local Government Association)
-
Jeremy Pocklington (Permanent Secretary, Ministry of Housing, Communities and Local Government)
-
Imelda Redmond (National Director, Healthwatch England)
-
Representation from the Care Providers Alliance
-
Simon Ridley (Director General, Cabinet Office)
-
Duncan Selbie (Chief Executive, Public Health England)
-
Kate Terroni (Chief Inspector of Adult Social Care, Care Quality Commission)
-
Chris Wormald (Permanent Secretary, Department of Health and Social Care).
Invitees (executives)
-
Professor Jane Cummings (Chair of Royal College of Nursing Foundation)
-
Ian Dodge (National Director for Strategy and Innovation, NHS England)
-
Catherine Frances (Director General for Local Government and Public Services, Ministry of Housing, Communities and Local Government)
-
Dr Eamonn O'Moore (SRO, Social Care Team, Public Health England)
-
Rosamond Roughton (Director General, Adult Social Care, Department of Health and Social Care).
Advisory groups
In order to utilise the widespread expertise in the sector, 8 advisory groups were established, focusing on key themes in social care, to widen the spread and depth of the advice. The advisory groups were asked to produce a short report for the taskforce Chair, by 7 August 2020 or later, by agreement.
The advisory groups were each supported by a policy lead from DHSC who could advise on developing and reporting the proposals. They were all asked to include people with lived experience in their work.
The advisory groups' chairs presented their key recommendations/advice to the taskforce. The advisory group reports are published alongside this overarching report and are an integral part of the work of the taskforce. Their recommendations are included in the list of recommendations in this report and some of their insights and analysis are threaded into this report.
The advisory groups (and their chairs) were:
-
BAME communities: Cedi Frederick (Chair, North Middlesex University Hospital NHS Trust) and Tricia Pereira (Head of Operations, Adult Social Care, London Borough of Merton)
-
carers: Emily Holzhausen (Director of Policy and Public Affairs, Carers UK) and Dame Philippa Russell (Carer)
-
good practice, guidance and innovation: Kathryn Smith (Chief Executive, Social Care Institute for Excellence) and Professor Robin Miller (Head of Department, Social Work and Social Care, University of Birmingham)
-
mental health and wellbeing: Kathy Roberts (Chief Executive, Association of Mental Health Providers) and Stephen Chandler (Director of Adult Social Services, Oxfordshire County Council)
-
older people and people living with dementia: Caroline Abrahams (Director, Age UK) and Kate Lee (Chief Executive, Alzheimer's Society)
-
people with learning disabilities and autistic people: Alex Fox (Chief Executive, Shared Lives), Trevor Wright (InSight Autism CIC) and Rachel Moody (Lived Experience Co-Chair)
-
self-directed support: Jenny Pitts (Programme Lead, National Development Team for Inclusion) and Dr Ossie Stuart (Trustee, Social Care Institute for Excellence)
-
workforce: Vic Rayner (Executive Director, National Care Forum) and Colin Angel (Policy Director, United Kingdom Homecare Association).
Approach
The taskforce team has worked intensively for the period from June 15 to August 28. Initially the focus was on establishing the detail of the taskforce objectives, with team members meeting on a daily basis to plan and implement the work of the taskforce, with a weekly review and planning meeting with a slightly wider set of specialisms. This work included representation from:
- DHSC
- Ministry of Housing, Communities and Local Government (MHCLG)
- Local Government Association (LGA)
- Association of Directors of Adult Social Services (ADASS)
- NHS England and Improvement (NHSE/I)
- Public Health England (PHE)
- provider services managers
The trade associations and the Care Provider Alliance were not only represented on the taskforce but contributed in facilitating support for the work.
There was weekly reporting to the Taskforce Accountability Group with the Minister of State and there were updates and a particular focus in weekly meetings on social care with the Secretary of State.
Key themes in the management of COVID-19 and social care
Personal protective equipment (PPE)
In the initial phase of the pandemic, significant concerns of the sector focused on accessing sufficient supplies of personal protective equipment (PPE) and the escalating costs of procuring PPE. Given the increased understanding of the risks associated with this particular virus, the guidance was reviewed and updated, regularly, leading to an increased need for and use of PPE.
The traditional route for the supply of PPE in the social care sector has been through wholesalers, with the costs met through local authority, health service and privately funded fee rates. The pandemic has led to an extraordinary level of usage and cost to local authorities and providers.
The taskforce reviewed the issues and considered the future supply and costs of PPE. The taskforce heard that, as a result of the work of Lord Deighton's Taskforce, the government is in possession of 4 months' supply of PPE, with confidence in the delivery of future contracts to supply the government until the end of the financial year.
We heard concern from the trade unions that some employers were not making available adequate supplies of PPE. We think the mechanisms for staff to raise concerns with local authorities and the CQC, having previously raised it with providers, should be clarified so that these matters can be investigated and resolved where necessary.
Local authority representatives believe that the costs of PPE have exceeded the level of financial provision made to the sector via local authorities. The supply and usage of PPE is fundamental to infection control in social care settings and provision.
Recommendation 1
Sufficient PPE provision to all social care providers (regulated and unregulated settings) should be made, free of charge, until at least the end of the current financial year (until 31 March 2021).
Consideration should be given to making a contribution to the costs of PPE, experienced by the sector in this financial year to date.
Action for: DHSC / Her Majesty's Treasury (HMT)
The taskforce recognises the contribution of wholesalers to the supply of PPE in the sector, so far, and the need to maintain these relationships so that, when the supply chain returns to normal, the wholesalers are in a position to respond to the needs of the sector.
Recommendation 2
Government to ensure that robust distribution mechanisms for PPE, for the sector, including emergency supply arrangements, are in place; and to communicate clearly to the sector these arrangements for this winter.
Action for: DHSC
Recommendation 3
Local authorities should establish mechanisms for supplying PPE to informal carers based on individual need.
Action for: Local authorities
Recommendation 4
Organisations should work to agree joint mechanisms for enabling staff to raise concerns about access to adequate supplies of PPE.
Action for: CQC and local authorities
Testing
The supply and administration of testing is fundamental to effective infection prevention and control. There is a need for regular testing of staff and residents in care homes and in other similar environments where personal care and support is provided and it is difficult to maintain social distancing. It is an essential part in providing confidence to the sector, the workforce, service users and the public.
Progress has been made with a testing strategy and testing capacity. There has been the roll-out of whole home care testing and this is due to be expanded to those in supported living, to those receiving extra care, and to facilities where the risk of transmission warrants regular asymptomatic testing.
Testing is available for agency staff ‒ it is important that we can be certain this is being carried out due to the risks identified of staff movement in care homes. Care providers have done much to reduce the use of agency staff but, given the risks of infection in different settings, further measures need to be taken to reduce the risks further.
The testing of other visiting professionals who frequently move between community and residential settings and provide care to residents is being piloted and evaluated and roll-out will be considered alongside other infection prevention and control measures to reduce the risk of transmission. We also suggest that the position of other visitors is kept under review. This includes CQC inspectors, where currently it is considered that, as they do not provide personal care and subject to maintaining social distancing and wearing the appropriate PPE, they do not need to be tested regularly.
It is also the case that, where there have been outbreaks or areas with higher levels of transmission, testing for the care sector has been prioritised including both care homes and other community services such as home care. This needs to continue.
We heard, consistently, of the importance to families of visiting their loved ones in care homes. Some family carers are regular visitors and would previously have spent extended periods with their family members. In some cases, they are an integral part of a care plan to maintain the safety and wellbeing of residents (for example, in case where residents are living with dementia).
We understand that weekly testing of all care staff provides particular challenges in ensuring that all care staff are tested in a timely manner. It is important that the Infection Control Fund money is used to ensure that staff who are not working on a particular day are paid for their time to travel in and receive a test. This sits alongside ensuring that staff receive full pay if they need to be isolated.
Recommendation 5
NHS Test and Trace should ensure the availability of detailed data on care home tests undertaken and the positive and negative results to local government, taking into account of the legal requirements of general data protection regulation (GDPR).
Action for: NHS Test and Trace
Recommendation 6
In areas of high prevalence and local outbreaks, testing of care staff should be a priority. It is also recommended that SAGE continues to review the evidence to consider whether community staff should be tested routinely. As testing capacity becomes available, the government should review the testing of care staff in the community. A priority for consideration is live-in care workers.
Action for: DHSC / SAGE
Recommendation 7
Testing of regular family visitors to care homes should be reviewed by SAGE considering risks associated with visitors, risks to residents of not being able to see their families and circumstances where relatives' care and support in the homes is an integral part of the care plan
Action for: DHSC
Recommendation 8
The testing of essential and regular visitors to care homes, such as CQC inspectors, should be kept under review
Action for: DHSC and NHS Test and Trace
Recommendation 9
Meeting the testing capacity (including asymptomatic testing) needs of the adult social care testing strategy (published 3 July 2020) should remain a first priority for the government. The strategy should be evaluated, in the autumn, as planned
Action for: DHSC
Recommendation 10
Outbreak management in care homes should remain a testing priority utilising 'pillar one'.
Action for: DHSC
Recommendation 11
All agency staff should continue to receive weekly testing and agencies should put mechanisms in place to ensure this is done. Government should put in place regulations to require providers to ensure staff have been tested before they work in a care home
Action for: DHSC
Flu vaccination
It has already been announced that flu vaccinations are to be supplied free of charge to all social care staff. Users of social care services are already a priority for flu vaccinations through primary care. Given the significant additional risk of COVID-19 this winter, the vaccination of all users of social care services, the workforce and family carers (unpaid) must be a major priority, to address the resilience and safety of staff and service users.
Over recent years, there has been a poor take-up rate for flu vaccinations within social care. It is essential that there is a concerted campaign to encourage uptake to ensure that all those working in social care are vaccinated. This will require very clear and targeted communication across the sector and a concerted effort by government, local authorities and providers. National monitoring should be established to enable government, local authorities and providers to understand how far this requirement is being met and where additional action needs to be taken.
In the NHS, staff can receive their flu vaccinations in the workplace. Every effort should be made to ensure that care staff can access vaccinations easily. All agencies must work together to maximise the number of eligible staff who receive the flu vaccination. This should include the training of peer vaccinators and visits by pharmacists to support workplace vaccinations, with the costs of administration being met through the Infection Control Fund.
The Advisory Group for People with Learning Disabilities and Autistic People advised of the need to work with self-advocacy groups, families and providers to ensure that people in this group, their family carers and support workers, receive flu vaccinations. This emphasises the need for flexible communication to reach particular constituencies with the social care sector.
Recommendation 12
Arrangements should be made, where possible, for workplace access to facilitate flu vaccination and other bespoke arrangements to ensure high take-up in the social care sector. This should include the training and deployment of peer vaccinators. There should be a local system in place to review progress and remove any barriers.
Action for: DHSC
Recommendation 13
There should be a national communications campaign to encourage take-up of the flu vaccination in the social care sector. This campaign should involve central government, local government employers and trade unions. It should cover service users, carers and the workforce
Action for: DHSC / local government / trade organisations and trade unions
Workforce and family carers
Infection Control Fund workforce measures
During the course of our work, we have heard about the extraordinary commitment of adult social care staff in trying to keep safe the people for whom they provide care. In some cases, care workers have locked themselves down in care homes and away from their own families to make sure they minimise the risk of transmission. There is also the unseen commitment from service users themselves and from family carers to keep going when more formal forms of support are restricted or unavailable. Around 1 in 5 of the care workforce are balancing their work with unpaid caring responsibilities. Supporting the care workforce with this balance can help with recruitment and retention.
This report and that of the advisory group includes a number of different recommendations relating to family carers without whom there would be greater challenges during this time. It is important that they are at the forefront of planning and delivery.
There was an increasing recognition among the public, in recent months, of the very significant contribution of the social care workforce and family carers as the understanding of their role and responsibilities grew. Social care is not as well understood as the health service. The steps taken to improve this understanding and recognition by government and the sector should continue as it is an important component in developing a sector that has confidence and resilience.
There are 1.5 million people working in social care, providing care and support in, or from, 38,000 settings. A total of 1.25 million people are in direct care roles. Of this group, 865,000 are care assistants. This group is mainly paid at, or close to, the Living Wage. There are 36,000 registered nursing jobs, 35,000 of which are with nursing care home providers.
During the last few months, vacancy rates have reduced from 8.1% (pre-pandemic) to 6.7%. Annual rates of turnover, the number of people leaving their job roles each year, are high. For care assistant roles in care homes, this stands at 40% per year. A total of 10% of care assistant roles in care homes are occupied by staff working on zero-hours contracts. In home care, 40% of jobs have zero-hours contracts. For care assistants in care homes, the latest data from Skills for Care surveys shows that the absence level of care staff in care homes is 9.6%. The overall terms and conditions have set the context for long-term recruitment and retention problems in the care sector.
Two workshops were held with a range of providers from the care home sector, including the Local Government Association and the Association of Directors of Social Services, to examine the issues associated with staff movement. This was as a result of research that demonstrated that homes whose staff worked in more than one setting were twice as likely to have an outbreak of the virus, among staff and residents, than those who had no staff working in other settings.
Similarly, the research demonstrated that there had been a lower level of outbreaks in homes where staff retained their full pay when absent through illness or as a result of isolating.
A full review of all the options considered is covered in the section on the Care Homes Support Plan. One option that was considered was banning staff movement, through additional legislation. However, providers were concerned that without improving recruitment and retention, it would not be possible to eliminate staff movement; and that attempts to do so would increase the risk of homes being unable to maintain safe staffing levels.
The recruitment and retention of home care staff has been a problem for a number of years. This is the major reason why the highest proportion of delays in transfers from hospitals is the level of home care service available.
Levels of absence, vacancies and turnover are the fragile workforce backdrop to the pandemic and a major risk in the second half of the year. These issues not only lead to a higher risk of infection, but also mean that capacity is at greater risk of being insufficient to respond to need during the height of the winter.
Based on data over the last 2.5 years from the Adult Social Care Workforce Dataset (ASC-WDS), completed by 55% of CQC-regulated independent providers, the care worker vacancy rate normally increases by between 0.5% and 1%, in winter and autumn months, compared to spring and summer. Assuming that this is representative for the whole workforce, this would equate to around an additional 4,000 to 8,000 care worker vacancies, due to winter pressures.
Clearly, a significant priority for government and the sector is to increase recruitment, reduce vacancy levels, reduce staff turnover and reduce staff movement between settings. In order to do this, we need to recruit more staff and improve levels of retention. This will require national and local campaigns.
The Workforce Advisory Group provided a particular focus on the actions required for the next phase. Their recommendations fall into a number of categories.
Within 3 months, they suggest government should instigate a review of employment terms and conditions in the sector. This is clearly a longer-term piece of work and consistent with a People Plan for the sector. The evidence from the taskforce review is that this would be an important initiative to ensure the resilience of the sector and the wellbeing of the workforce in the future. It has been strongly supported by members of the taskforce.
There is another set of recommendations which relate to maintaining the wellbeing of the workforce - related to adequacy of supply of PPE, testing, and workers who have been shielding. These are picked up in the recommendations contained in this overarching report.
Finally, the advisory group refers to the need to do further work to address short-term workforce capacity. This, together with measures to retain experienced members of the workforce, should be reviewed through the development of a short-term workforce plan. The particular issues for further review are:
-
workforce retention over the winter
-
nurse returners and nurse students
-
upskilling the workforce
-
managing any recruitment issues arising from the European Union exit
-
maximising the effectiveness of COVID-19 workforce initiatives.
Spotlight: Supporting recruitment in London
Five councils in the North London Sustainability and Transformation Partnership (STP) launched a Proud to Care London recruitment website in June 2019.
The website is a free-to-use online recruitment portal for care providers and showcases jobs in north London, the wide range of career pathways available and case studies, to increase recruitment and retention into the sector.
Recommendation 14
The government should set up a short-term workforce planning group to further address workforce capacity issues, likely to arise over the next 6 months. To conclude its work within 6 weeks.
Action for: DHSC
Recommendation 15
Government should keep under review vacancies and absence levels and consider further measures to improve recruitment and retention if existing strategies do not sufficiently fill the gap. This should include the continuation of recruitment marketing to attract the right candidates to fill existing vacancies.
Action for: DHSC
Recommendation 16
There should be a review of the access to support available to social care staff, in particular for wellbeing services.
Action for: DHSC
Training
This report highlights the training on infection prevention and control provided by the NHS and that this offer of support continues to be available via the NHS. The importance of continuing to invest in and find ways to make it available to the workforce is critical to the confidence and resilience of the workforce.
Spotlight: e-learning for staff in Lincolnshire
There is an established programme of training and support to care homes in Lincolnshire for infection prevention and control, provided by the council's health protection team and Lincolnshire CCG's health protection nurses. As part of the response to COVID-19, the team has produced a suite of resources including audit templates and care plans templates, and has supported care homes through the interpretation of national policy and produced local guidance. To support staff understanding of the COVID-19 virus, e-learning modules were developed and made available on in March 2020, covering awareness and infection and control, and managing the signs and symptoms for health and social care workers. To date, more than 1,000 care workers have undertaken the e-learning.
Providers report that, in response to COVID-19, care staff have been asked to complete tasks that were previously undertaken by community health workers. A robust system needs to be put in place to ensure that care workers who carry out these tasks are trained properly, in order that the health and safety of care recipients and workers is protected. The tasks need to be kept under review to ensure that funding is made available from health to social care, where this reflects a transfer of responsibility
Recommendation 17
There should be appropriate training and support agreed and provided for care staff who are undertaking delegated tasks.
Action for: DHSC / Skills for Care
Funding
The overall funding and sustainability of the sector are out of scope of the taskforce. However, this is being kept under review separately by the Department and Ministers. One issue we need to address is the 'cliff edge' when additional funding and payments in advance finish and a switch to retrospective payments is made. However, the Infection Control Fund (ICF) and the supply of PPE, are inextricably linked to both the impact of COVID-19 and safety - and are major costs to the sector.
The Infection Control Fund was introduced alongside the Care Homes Support Plan in May 2020. The taskforce provided advice to the government as to whether the fund had been effective and should continue. Funds were granted on the condition that local authorities passed at least 75% directly to providers, on a per-bed basis, in accordance with grant conditions, irrespective of the funding source for the fees, and on the basis that COVID-19 is a significant risk to all residents and care home settings. The remaining 25% was to be used at the discretion of local authorities in line with the grant conditions, in any part of the social care sector, focused on the workforce and infection control. This could be used in other parts of the sector such as home care. Otherwise, the grant conditions were to:
-
ensure that staff who are isolating, in line with government guidance, receive their normal wages while doing so. At the time of issuing this grant determination, this included staff with suspected symptoms of COVID-19 awaiting a test, or any staff member for a period following a positive test
-
ensure, so far as possible, that members of staff work in only one care home. This includes staff who work for one provider across several homes or staff that work on a part-time basis for multiple employers and includes agency staff (the principle being that the fewer locations that members of staff work the better)
-
limit cohorting staff to individual groups of residents or floors/wings, including segregation of COVID-19 positive residents
-
support active recruitment of additional staff if they are needed, to enable staff to work in only one care home, or to work only with an assigned group of residents or only in specified areas of a care home, including staff who have chosen to temporarily return to practice, and those returning through the NHS returners' programme. These staff can provide vital additional support to homes and underpin effective infection control while permanent staff are isolating or recovering from COVID-19
-
limit the use of public transport by members of staff. Where they do not have their own private vehicles, this could include encouraging walking and cycling to and from work, and supporting this with the provision of changing facilities and secure bike storage or use of local taxi firms
-
provide accommodation for staff who proactively choose to stay separately from their families in order to limit social interaction outside work. This may be provision on site or in partnership with local hotels
There were concerns about a risk that state aid might apply and this, in turn, led to a level of scrutiny and specificity in the application of the grant that attracted some criticism from local authorities and providers. There is a view from some (not all) providers that the grant methodology has led to more of the funding being accessed by providers, compared with the grants that had been given previously, to local authorities, for social care and other council functions. It is inevitable that the delivery of a generic grant will be applied on a discretionary basis by local authorities across a range of council functions through a need to address several priorities, of which, adult social care is one.
In view of the government's intention to achieve specific outcomes from this policy objective (even though there may be some variation in local areas about ways to achieve this), it is appropriate that money should be targeted on specific measures. In this case, it refers to measures that reflect the evidence from national and international research and best practice on infection, prevention and control.
The provisions of the grant were informed by Scientific Advisory Group for Emergencies (SAGE) advice on the risks in the care sector. In the meantime, our understanding and knowledge of the science of how the virus works, its impact on people who use social care services in the places they live and receive care and support, has grown. It is also the case that, as general lockdown relaxations are implemented, new requirements come to the fore. It is, therefore, appropriate to review and take stock of the conditions attached to the grant.
The ICF was designed to help local areas to develop their plans and to encourage the completion of information by providers so that there could be more clarity on the degree to which providers were able to implement the measures identified in the Care Homes Support Plan.
The tables below show the improvement in several measures of between 10% and 45% over the life of the Care Home Support Plan and the ICF. This data in the tables is from the capacity tracker and was downloaded on 10 August 2020
Alongside the provisions of the Care Home Support Plan, the ICF has acted both as a tool and a lever, to reduce the risk of outbreaks. The table below demonstrates this, with the completion of information increasing from 45% to 99%. This level of data collection is helping Ministers, the DHSC, the taskforce, and local systems and partners to achieve much clearer analysis and action at a regional and local level.
Proportion of care homes responding 'yes' to infection control measures
Focus 1: infection prevention and control measures
| 29 May 2020 | 10 Aug 2020 | Change (percentage points) | Response rate from care homes, 10 Aug | |
|---|---|---|---|---|
| 1.1. Ability to quarantine/isolate/cohort when needed | 81% | 94% | 13 | 94% |
| 1.2. Actions to restrict staff movement between care homes | 78% | 92% | 14 | 92% |
| 1.3. Paying staff full wages while isolating following a positive test | 37% | 68% | 31 | 68% |
Focus 2: testing
| 29 May 2020 | 10 Aug 2020 | Change (percentage points) | Response rate from care homes, 10 Aug | |
|---|---|---|---|---|
| 2.1. Registration on the government's testing portal | 66% | 94% | 28 | 94% |
| 2.2. Access to testing for all asymptomatic residents and staff | 34% | 82% | 48 | 82% |
| 2.3. Testing of all residents discharged from hospital to care homes | 63% | 83% | 20 | 83% |
Focus 3: personal protective equipment (PPE) and clinical equipment
| 29 May 2020 | 10 Aug 2020 | Change (percentage points) | Response rate from care homes, 10 Aug | |
|---|---|---|---|---|
| 3.1. Access to sufficient PPE to meet needs | 86% | 99% | 13 | 99% |
| 3.2. Access to clinical equipment needed for COVID-19 | 72% | 86% | 14 | 86% |
Focus 4: workforce support
| 29 May 2020 | 10 Aug 2020 | Change (percentage points) | Response rate from care homes, 10 Aug | |
|---|---|---|---|---|
| 4.1. Access to training in the use of PPE from clinical or public health staff | 82% | 94% | 12 | 94% |
| 4.2. Access to training on the use of key medical equipment needed for COVID-19 | 66% | 79% | 13 | 79% |
| 4.3. Access to additional capacity including from locally co-ordinated returning healthcare professionals or volunteers | 50% | 66% | 16 | 66% |
Focus 5: clinical support
| 29 May 2020 | 10 Aug 2020 | Change (percentage points) | Response rate from care homes, 10 Aug | |
|---|---|---|---|---|
| 5.1. Named clinical lead in place for support and guidance | 59% | 85% | 26 | 85% |
| 5.2. Access to mutual aid offer (primary and community health support) | 81% | 94% | 13 | 94% |
Recommendation(s) 18
In view of this and the continued threat of the pandemic to care homes and the wider social care sector, our recommendation is that the Infection Control Fund should be in place for the rest of the financial year. The conditions which led to the provision of the grant still exist and will do so for the remainder of the financial year at least. In addition, we would recommend:
-
rollover of any unspent committed funding for use in the rest of the year. The impact and response to COVID-19 was immediate and unpredicted. Providers and local authorities had to understand what action they needed to take. It clearly took some time for local providers to determine what changes they needed to make and how the grant would be aligned. There is also feedback that the short-term nature of the grant led to some reluctance in applying some measures, including paying full pay while staff were isolating or absent through sickness
-
specified funding for the rest of the social care sector to enable all staff to self-isolate or to be absent through sickness without losing pay. The proposal here is to use a model deployed by Hertfordshire County Council, which provided an allocation based on the number of service users in home care, utilising self-directed support and supported living
-
use of the funding to support extra staff and equipment to manage the new visiting policy safely and effectively
-
reinforcing the existing conditions, including the ability to employ extra staff or increasing pay to meet the requirements of reducing staff movement, or supporting residents who need extra support to remain socially distanced from others
-
local authorities creating a staff bank to deploy people into the care sector on a placement basis, with appropriate testing and isolation procedures in order to reduce staff movement, responding to any staffing shortfalls as a result of recruitment challenges, or resulting from infection. This would include any costs associated with indemnity. It would include arrangements for the supply of nurses in conjunction with local health services or the returners and young professionals scheme
-
allowing spending on equipment and technology to aid infection control
-
allowing payments to offset reduced occupancy where this is required in order to implement appropriate/cohorting/zoning of residential establishments and staff groups in line with Taskforce recommendations (soon to be available). This includes, for example, the provision of separate rooms for changing into and out of PPE and the storage and retrieval of supplies
-
enabling use of up to 10% of the funding for PPE. The government is keeping under review the provision of free PPE to the sector. This would allow some flexibility in meeting the costs of this very important equipment. However, if the government does, as recommended, make free PPE available for the rest of the financial year with some support for costs incurred, this provision would be unnecessary
-
given the evidence of the link between paying staff full pay to isolate or absent through illness, the government should make the availability of the future grant subject to full pay to ensure that is carried out across the sector during the pandemic
-
DHSC should consider an increased respite offer to informal carers. This should sit alongside a campaign for carers, recognising their challenges and encouraging options for them to consider a break
Actions for: DHSC
The extra costs of insurance, during this financial year, were considered – DHSC has advised that this will be kept under review by other means.
The Local Government Association has proposed a decrease in the level of the grant that is passed directly to providers, to 50%, on the basis of increased flexibility to deploy the money, based on greatest need and risk. Providers tended to support specific allocations to care homes and the community care sector rather than the flexibility suggested by local government. Clearly, the proposal above to specify an amount for the rest of the sector, in addition to care homes, could potentially reduce flexibility. However, the resilience of services providing care for people in their own homes will be critical during this period of heightened risk, particularly given the number of people who require care at home having left hospital or due to increasing needs while living at home.
Another proposal was a request for further guidance through the Local Government Association on the application and monitoring of the grant in order to achieve greater consistency across the country. A further issue raised by both providers and local government is the uncertainty and administrative burden of the current funding coming in 2 tranches. The government should consider reviewing this position and lengthening the period between payments.
Evidence and guidance
Throughout the pandemic there has been a need to develop, rapidly, guidance based on increased understanding of the nature of the virus. Most of this has been developed by Public Health England and increasingly with detailed consultation and engagement with the sector. It is of critical importance that the guidance is developed with the benefit of expertise from the sector. In an emergency, this requires speed and agility in government and in the sector, to ensure this is done with both technical and scientific expertise, and jointly with those who need to implement and adhere to the resulting guidance.
This rapid development led to regular revisions of the guidance which led to some providers expressing the view that the guidance could appear contradictory or difficult to access and interpret in a timely manner. Steps have been taken to address this by using different formats for the presentation of the guidance and having one site where the guidance can be found. It remains critically important that guidance is, as far as possible, co-produced with the sector. The Advisory Group for People with Learning Disabilities and Autistic People emphasised the importance of accessible guidance and communications for people in this group and their families being issued with or very soon after all future COVID-19 guidance.
It is also important that the frequent publication of evidence across the world about COVID-19 is taken into account in formulating policy and best practice across the sector. The taskforce has regularly reviewed the evidence available which has informed this advice and recommendations. The Guidance, Good Practice and Innovation Advisory Group proposed undertaking a review of good practice globally for innovation in social care. The International Long-Term Care Policy Network provides regular updates on research and evidence from across the world. The taskforce welcomes the establishment of a SAGE care homes sub-group and recommends that this continues, with its wider brief for the social care sector as a whole. It would be able to give specific advice on requests to government and the sector, and review existing evidence on transmission, mortality and best practice. It would make further recommendations about further measures that should be put in place to protect people from the virus and take into account other factors that affect wellbeing and all-cause mortality rates. This includes specific information that is available for particular groups of people who receive health and care support.
The Guidance, Good Practice and Innovation Advisory Group make a number of important and helpful recommendations relating to guidance that need to be accommodated in conjunctions with the recommendations below.
Spotlight: New guide on infection control in the North West
The directors of adult social services (ADASS) in the North West have produced an informative top tips guide to care home infection control. The guide highlights some of the ways in which residential and nursing homes have responded to the COVID-19 pandemic in order to ensure the safety of residents in very challenging and difficult circumstances. A range of case studies are included in the guide including using motor homes for additional sleeping capacity for staff, turning a large room into a 'flat' for a person living with dementia, or using different coloured t-shirts to help staff work in new teams.
Recommendation 19
DHSC should ensure that there is an easily accessible central site for all social care guidance relating to COVID-19, produced in a range of accessible formats. The site should provide links to supplementary evidence.
Action for: government communications
Recommendation 20
Government should ensure that all guidance is developed with the sector in all cases and protocols developed for ensuring that this is undertaken efficiently and effectively
Action for DHSC
Recommendation 21
It is recommended that the SAGE sub-group has a wider brief for the social care sector as a whole.
Action for: Deputy Chief Medical Officer
Communications
In any crisis situation there is a need for excellent communications to:
-
inform - provide timely and relevant information about the changes in the situation, nationally and locally, so that people are aware of the context and risk levels
-
assure - provide appropriate guidance that enables people to take timely and appropriate action to keep themselves and others safe
-
inspire - maintain the community spirit, recognise the personal hardships faced, and validate the extreme efforts and personal sacrifices that people take to protect the lives of those around them
Throughout the period of the taskforce, we always recognised the challenges of the complexity of risk in social care and the diversity and distributed nature of the sector. Specifically, we must increase the level to which we inform the sector about the risks and issues arising from the changing levels of transmission and risk, in different places, so that social care managers and informal carers can make judgements about appropriate behaviours on a day-to-day basis, in their area.
We must also find a different way to assure ourselves that appropriate actions are being taken. There are various infection control measures that individuals and organisations can take and new best practice for settings emerges regularly as creativity and innovation flourishes in the sector. We need to encourage and provide channels for sharing best practice and find solutions to the communication challenges. Government must present information, guidance and advice in different formats for different audiences, accessibly and using appropriate language for the sector or group. Guidance needs to be made accessible in an easily findable and ordered one-stop shop with minimal duplication, version control, and clear labelling by audience.
Finally, we must redouble our efforts to inspire the sector. We must recognise the sector's heroic efforts and demonstrate the national understanding of the sector and what it has delivered. We must amplify the voices of the local heroes who have relentlessly protected the most vulnerable on the frontline at such a dangerous and isolating time. This recognition must also include the efforts of formal and informal care, including the efforts of volunteers and particularly carers who have faced increasing care responsibilities while, in certain cases, receiving less of the support they themselves may have been accessing pre COVID-19.
Recommendation 22
A social care specialist should be included in developing communications in a range of accessible and culturally accessible formats including guidance aimed at unpaid carers at national level to reflect the specific challenges and achievements of the sector.
Action for: DHSC
Recommendation 23
Create a digital space where guidance is easily navigated and accessible to all aspects of the social care system in a simple format. Within this space, create a place to amplify the voices of the sector, share best practice and recognise heroic efforts.
Action for: DHSC
Recommendation 24
Local systems are recommended to establish a weekly joint communication from local directors of adult social services and directors of public health to go to all local providers of adult social care as a matter of course through the winter months.
Action for: Directors of adult social services
Recommendation 25
There should be a single dashboard which can be used by each region for the social care sector based on the national dashboard, and used to identify risk and support improvement.
Action for: DHSC with local government / ADASS / Directors of public health / provider representatives
Clinical support
Clinical support to care homes
Evidence from the enhanced care in care homes initiatives, in recent years, is that the support of a clinical lead, in regular contact with a care home, establishes a detailed working relationship with the care home. The clinical lead can provide advice, guidance, assessment and treatment to residents, leading to better outcomes. This is an integral part of an effective health and social care service to residents and their family carers. This support can help avoid the traumatic experience of attending accident and emergency and some hospital admissions. Of course, where necessary, hospitals are the best option for providing the expert emergency treatment that people need. The provision of a clinical lead was agreed as the Care Homes Support Plan was being launched. The NHS has announced that the enhanced care in care homes initiative will be rolled out, across the country, by 1 October. In order to take full advantage of this comprehensive approach to all 15,500 care homes across the country, there needs to be information provided to the care sector about the clinical support role, what each home can expect and their responsibilities in receiving this service.
Spotlight: Improving primary care support for care homes in West Yorkshire
The Five Lane Primary Care Network in Bradford, West Yorkshire, has aligned local care homes to the 4 GP practices in the network to improve continuity, reduce social contact and build a better relationship with the care homes. While this approach is embedded in the new GP contract, the partnership took this action independently on its own initiative in response to COVID-19. It has received very positive feedback from care home managers. Many residents at the care homes were registered under the care of doctors at another practice, so the partnership consulted with those practices, and residents and families. The partnership asked for the care homes' help in discussing the transition with patients and relatives to seek consent and created a letter for relatives to explain the reasons and ask for their approval. The change also found approval with the local district nursing team, which is based in the same building as the partnership. Since lockdown, as well as being available for urgent calls, GPs at the partnership have dedicated time every Thursday morning to perform a ward round of the residents (either telephone, video or face-to-face as needed). This step has significantly improved patient care, professional to professional relationships, networking and medicines management.
Recommendation 26
Communicate the aims and best practice for the clinical lead role for care homes, along with advice on how they maximise the value of their clinical lead. Put into place visible arrangements locally and nationally for assuring that a clinical lead remains in place for each care home.
Action for: NHSE / CCGs / Primary care networks
Recommendation 27
Primary care networks and community health services should ensure that a weekly review in care homes is undertaken including structured medication reviews. Care homes should work with the local multi-disciplinary team to ensure this works effectively.
Action for: Primary care networks, community services and multi-disciplinary teams
Recommendation 28
Communicate to providers a clear plan, with timescales, for the implementation of the Enhanced Health in Care Homes programme, detailing what support providers can expect to be in place and what preparations they should be making.
Action for: NHSE / CCGs
Recommendation 29
Local systems should engage with local care providers to implement monitoring and video conferencing tools for increased access to GPs/primary care.
Action for: Local authorities and CCGs
Recommendation 30
Directors of nursing in CCGs to provide professional leadership and expert advice on infection prevention and control in local areas to support the local authority and directors of public health in discharging their responsibilities.
Action for: NHS / CCGs
Clinical support for people living at home
The NHS Long Term Plan set a clear ambition to boost out-of-hospital care and improve the links between primary and community health services. Building on learning from integrated care 'vanguards', it committed to adopting models of proactive identification, assessment and support for patients at high risk of losing their independence.
One such model is anticipatory care, which introduces more proactive, co-ordinated care for patients assessed as being at high risk of poor health outcomes. This approach also helps avoid admissions to hospital. The NHS is moving towards implementation of this approach in 2021. In the meantime, it is advised that Sustainability and Transformation Partnerships and Integrated Care Systems engage with providers of 'care at home' (primarily domiciliary care, personal assistants/supported living agencies) to meet the healthcare needs of the people they support as part of their approach to population health management.
The Guidance, Good Practice and Innovation Group has recommended that best practice in this area could be supported by some guidance co-produced with the NHS Confederation Primary Care Network and the Royal College of General Practice (and we would wish to see nursing and wider multi-disciplinary teams included too).
Recommendation 31
STPs and ICSs to ensure that, through their approaches to population health management, primary care networks ensure that the risks and needs of users of social care services in the community are identified and reviewed.
Action for: STPs and ICSs
Movement of people between care and health settings
A longstanding challenge of the health and social care system is the ability to transfer people from hospital to alternative health and care settings. The evidence is that extended hospital stays are not usually the best way for people to recover or to regain as much of their health and wellbeing as possible.
One policy developed in social care has been 'discharge to assess'. Extension of the model requires funding for payment of up to the first 6 weeks of social care and integrated working between health and social care. It is essential that hospitals ensure that providers have enough information with which to meet the needs of service users and that the requirement for testing of people who are discharged from hospital to care homes is met and communicated to the care home in advance, in each and every case. The evidence is very clear that enabling people to leave hospital as soon as possible is in their best interests while, of course, ensuring that it is safe to do so. The principle of this model is that, wherever possible, people should be provided with enough support to go 'home first'. Where health and social care work intensively together (to provide reablement and rehabilitation) to support people in the community, the evidence is that the outcomes for people can be very good.
The current policy is that all people who leave hospital for a care home should have been tested and results shared in advance of discharge. This policy was agreed with the Chief Medical Officer in April 2020. The taskforce Chair has asked the Deputy Chief Medical Officer, in her capacity as the chair of the SAGE sub-group for care homes, to review the evidence of risk and, as necessary, make further recommendations to government as a result. This matter was also raised by ADASS. At the same time, ADASS were asked to lead work with the sector to develop appropriate cohorting and zoning practice. The SAGE sub-group will therefore undertake a review of the data and evidence and will commission further work including relevant studies. The result should be available in mid-September 2020.
Recommendation 32
The SAGE sub-group to review the evidence on the risks associated with the discharge of COVID-19 positive people from hospital and admissions of COVID-19 positive people from the community to care homes.
Action for: SAGE sub group
Inspection and regulation
Overview
The Care Quality Commission (CQC) recognised the intense pressure on health and care providers during the COVID-19 pandemic, and the increased risks to staff and people who use services, whether they had tested positive for COVID-19 infection or not. In March 2020, they paused their routine inspection programme but maintained their regulatory role and core purpose. Keeping people safe has been the priority.
Supportive and problem-solving conversations with providers
The CQC developed its Emergency Support Framework (ESF) ‒ a structured framework for the regular conversations they have with providers, adapted to the specific needs of each sector. CQC's conversations with providers have focused on 4 areas:
- safe care and treatment
- staffing arrangements
- protection from abuse and protection of human rights
- assurance processes, quality monitoring and business risk management
The assessments help CQC to understand how providers are managing, and whether any additional support is required. By 3 August 2020, CQC had completed 14,884 ESF assessments of 14,232 individual adult social care locations.
As referenced by the Secretary of State for Health and Social Care in a 2020 speech on the future of healthcare, the ESF represented an adaptation of CQC's usual regulatory approach to the new reality. It used data and feedback to identify problems in real time, worked with providers to have honest conversations, and offered ongoing advice and support. It also introduced a new home care tracker, designed to work alongside the NHS Tracker for adult social care, to help us monitor risks to the quality of care. The CQC has heard, through its engagement, that providers have valued the supportive role CQC has played alongside their regulatory role during the COVID-19 pandemic.
Using intelligence to keep people safe
CQC wants to be smarter in how it regulates, by making its approach simpler and more dynamic to reflect ever changing services. It will build on its work to be intelligence-driven, be more effective and more efficient. This means using intelligence in a smart way to tailor and target actions where they will have the biggest impact. On-site inspections are a crucial tool and one that CQC will continue to use. Where CQC has information that people are not getting good care, a visit is often the best way to understand what is happening. Alongside this, it will continue to use and develop its monitoring tools, using the learning from the response to COVID-19 to develop the way that it regulates so it can support providers to provide the best possible care.
CQC's experts by experience have continued to support domiciliary care inspections by speaking to people who use services and their families on the telephone. CQC is planning to pilot how its inspectors and experts by experience can speak to people who use services, their families and local community and advocacy groups, using virtual methods.
Highlighting best practice through inspections
In consultation with the taskforce chair and with the agreement of the Minister of State, CQC has been working to identify and share best practice with providers on infection prevention and control (IPC) and has been undertaking inspections specifically related to IPC across a sample of 300 care homes where their intelligence indicates providers have managed IPC well. This includes services which have had an outbreak and reviewing how they were managed, alongside services that have remained COVID-19 free. Feedback from the initial inspections has identified some good practice examples. CQC's initial findings will be shared in September 2020 as part of its regular COVID-19 Insight reports, with a wider set of findings to be shared in the November edition.
To do this, it developed a new IPC inspection tool, with questions and prompts, which will be used for this IPC review and on all upcoming inspections of care homes. This will be published on CQC's website, and in the future, it will explore how it can be adapted and used in other care services. The tool will help CQC to be assured that people are receiving care which is underpinned by safe, high quality IPC. In addition to the IPC inspections, CQC is highlighting best practice by publishing innovative examples of how providers are responding to the pandemic on its website.
Provider collaboration reviews
This rapid piece of work has involved engagement with partners and analysis of CQC's data and intelligence in order to review how providers are working collaboratively in response to the pandemic. To date, it has undertaken reviews in 11 health and social care areas focusing on the over-65 population to understand the journey for people with and without COVID-19 across health and social care providers, including council and NHS providers and the independent sector. The reviews include experiences of people who use services.
CQC will be publishing some headline findings in its Insight report in September 2020 and a more detailed overview will be provided in CQC's State of Care report in the autumn. The findings will be structured around 4 key lines of enquiry, including:
-
people at the centre ‒ in responding to COVID-19, how have providers collaborated to ensure that people moving through health and care services have been seen safely in the right place, at the right time, by the right person?
-
system leadership ‒ was there a shared plan and system-wide governance and leadership during the COVID-19 period?
-
workforce capacity and capability ‒ is there a strategy for ensuring sufficient health and care skills across the health and care interface?
-
digital solutions and technology ‒ what impact have digital solutions and technology had on providers and services during the COVID-19 period?
CQC commissioned this work in order to support systems and providers by sharing learning and best practice from those areas where providers are collaborating well across boundaries, ahead of any potential 'second wave' of the virus, and also ahead of winter pressures. In October 2020, it will carry out fieldwork for a further 8 areas, with a focus on urgent and emergency care.
The pandemic has affected a range of different groups and future work may cover other people impacted by the virus, for example, BAME populations, carers, people living with cancer, children and young people, people with a learning disability and/or autism, people with mental health needs and those with long term conditions such as diabetes. CQC's ambition is to look at provider collaboration in all integrated care system/sustainability and transformation partnership areas and this will allow CQC to signpost the different waves of impact.
Local systems reviews
In 2017 to 2018, CQC reviewed health and social care systems in 20 local authority areas to find out how services were working together to support and care for people aged 65 and older. The 20 areas they reviewed were identified by DHSC and MHCLG based on a dashboard of metrics. These metrics, which were developed and agreed by the Secretaries of State, indicated challenges with access and how people move between health and social care services (including delayed transfers of care).
CQC remains committed to delivering local system reviews (LSRs) in the future. The previous LSRs and their thematic reviews over the years have showed that when local health and social care providers work well together, how people experience care can be significantly improved and costs can be reduced.
CQC is keen to undertake further LSRs given the positive impact the first programme had and the benefits that providers said they delivered for them. There is a balance to be struck between undertaking reviews, set against the overall demands of responding to the pressures this winter, which needs to be kept under consideration.
Recommendation 33
The CQC inspection framework should be reviewed to take into account the recommendations in this report and the winter plan.
Action for: CQC
Capacity, expertise and information
During the taskforce's work, there were a number of references to the need to ensure that, despite the different size and structures of the NHS and social care there should be equal consideration of the resources, policies and strategies in government. The Departmental role, in relation to social care, prior to the pandemic was focused largely on providing policy support to Ministers. The overall responsibility for commissioning of state funded services rests with the local authority and the statutory role of directors of adult social services. The NHS also commissions some social care services jointly with the local authority, or where the local authority takes a 'lead commissioning' role. A significant proportion of people (approximately 50% of those who are in residential or nursing care or 30% of those who receive community services) fund themselves. Directors of adult social services have an overarching responsibility for the market but (except in circumstances of providers exiting the market) no financial responsibility for self-funders or, normally, the element of the market.
The pandemic created unique and significant challenges in the context of a very diverse and distributed system. With rapid policy development requiring simultaneous interpretation and operational implementation, the taskforce was built with policy makers, local authorities, providers, public health and NHS involvement.
This team at a national level has been supported by a regional infrastructure from ADASS, the Local Government Association, and the Better Care Fund Team, working with Public Health England, the Association of Directors of Public Health and providers. This infrastructure has provided support and advice to local systems and has also enabled communication and assurance to take place between local and national levels, for example, on action in response to local outbreaks. Resources for improvement and support have, in great part, been re-purposed to meet challenges from the COVID-19 emergency. This provides a route into implementation of Taskforce recommendations.
In a national emergency, with rapidly increasing risk, the importance of clear data and information to drive policy and decisions about actions and resources is essential. There is a need to understand this information for assurance and to ensure that there is proportionate interest and intervention at a national level (in instances where this is required). It also provides the intelligence by which rapid policy changes and resource decisions can be made based on the evidence. Equally, at a local level, some local authorities, in conjunction with other local organisations (particularly the NHS) have good information but this is inevitably a mixed picture across the country. For the purposes of managing the implications of the circulation of the virus, it is imperative that data and information from different sources, including public health, NHS, CQC, local government and providers is brought together so that it can be interrogated rapidly and appropriate local action can be taken together. The information needs to be used for strategic and operational purposes at national, regional and local level.
The creation of the taskforce provided the ability to create a team drawn from the different constituencies of the sector, working together daily to deliver the taskforce objectives, develop new approaches and rapidly translate policy into implementation in local services. There are several cross-government forums for managing COVID-19 and during this period the taskforce Chair has represented social care. This was partly due to the desirability of having representation for social care from somebody who has substantial operational experience. There is a need for the government to have a team of subject experts drawn from across the sector working with policy leads and arm's-length bodies to develop guidance and initiatives, implement policy and develop implementation and delivery plans in partnership with the sector. This would also assist in providing leadership in government for social care in partnership with the sector.
Recommendation 34
It is recommended that DHSC significantly boosts its own expertise and capacity, in relation to social care, for the duration of the pandemic and beyond. It should do this by bringing in, perhaps through secondment, senior local authority figures with current/recent experience at senior levels both within social care and public health. Such expertise, allied to the soon-to-be-appointed Chief Nurse, could, for example, be deployed, during the pandemic, on the understanding and effective management of local COVID-19 outbreaks, with a role in linking effectively with regional and local structures. Looking more broadly, it is recommended that DHSC should consider what role a group similar to the taskforce could play in:
-
providing professional advice to DHSC policy officials, on the basis of interaction with the system, playing a key role in informing its development
-
continued implementation of the Care Home Support Plan
-
implementation of the adopted Taskforce recommendations
-
oversight of the quality and effectiveness of national policy through working in partnership with regional and local structures
-
supporting implementation/delivery – advising/supporting as well as identifying places where there are higher risks on a range of adult social care delivery issues
It is further recommended that these national level arrangements continue to be supported by a robust, resilient and agile regional structure which can support a line of sight at a national level into local situations, enable 2-way communications between local and national, and can deploy rapid and targeted support to local systems.
Use of data and digital
One of the biggest challenges facing the country and the social care sector, while responding to its biggest public health crisis for more than 100 years, is the availability of timely and reliable data and information. The scale and speed of change of transmission of infection and its impact has been, and remains, dramatic. This requires pulling data from previously disparate disciplines and sources and bringing them together in order to see the whole picture, helping to manage the implications of the pandemic at local, regional and national level. Ministers and policy makers need good, reliable data on which to assess risk, draft policy and develop appropriate interventions. Similarly, while regional and local systems have developed some good systems, the picture is inconsistent and comparisons are difficult to make. The Capacity Tracker, which has emerged as a major source of information during the pandemic, had a low response rate which improved significantly with the advent of the Infection Control Fund.
The taskforce has begun the process of building a new national social care dashboard for COVID-19. It is essential that this work is completed, with the data from various sources being made available on a timely basis for national and local bodies, commissioners and providers. This would see data integrated across government, CQC, Public Health England, NHS and the Joint Biosecurity Centre to provide the national COVID-19 social care dashboard.
For care settings, the continued improvement of Wi-Fi access and technology to enable to remote consultations, enhancing the homes efficiency and enabling the important connections between residents and family and friends virtually have become ever more pressing and important. We would encourage providers to invest, where appropriate using the Infection Control Fund. It is an important basic step.
Spotlight: Data dashboard providing COVID-19 overview in the West Midlands
Health and care colleagues in the West Midlands have used the ADASS COVID-19 dashboard to help their response to the pandemic. It curates relevant content from a range of published datasets to present a holistic view of risk and opportunity during the crisis and into recovery. The dashboard forms part of the region's growing data and knowledge hub and enhances 3 key capabilities - increased awareness, evidence for assurance, and facilitating action and support. The dashboard combines mortality data (ONS), tracker data (LG Inform), outbreaks information (gov.uk) and active locations from CQC data. The COVID-19 dashboard has helped identify areas of risk and take a balanced approach in enquiries made to local authorities.
Recommendation 35
The government to complete urgently the national COVID-19 social care dashboard.
Action for: DHSC
Recommendation 36
The DHSC must make some infrastructure changes in order to be able to address these data issues. Principles that should underpin this are:
-
robust data capture – capture once, use multiple times, and ensure that it is clear why data is needed and how it is being used so that good data quality is incentivised. Ideally this would see the establishment of a social care data source, rather than reliance on health or other platforms
-
rigorous database management – collating, cross-checking and processing data from multiple sources and organising it to be used consistently in ongoing reporting and ad hoc analysis
-
operationalising the data – getting the prioritised insights back to users immediately so they can address both emergent issues and data quality, driving proactive improvement. This will help support the sector with problem-solving and managing the pandemic
-
accessibility and democratising data – make both analysis and raw (or appropriately aggregated) data available to everyone as appropriate to their role in supporting the system. This one version of the truth can help to unite a distributed sector behind a shared understanding of where problems lie and what good standards look like
-
operational data leadership – establish the capability and capacity to set new standards of how data will be used to inform decision making. Driving both high standards around the collection and management of data and the active use of data operationally to inform priorities and interventions
-
governance and communication – establish clear roles and responsibilities for who takes which actions and how the data supports them to do so in a prioritised way. Ensure data provides a way to focus on what each part of the system can do and where more complex or multi-disciplinary work may be needed to investigate beyond the existing data
Action for: DHSC with support from across government
National, regional and local structures
COVID-19 places particular demands on public services in ensuring there is sufficient capacity and capability to protect the public while at the same time enabling people to carry on with their lives as much as possible, maintaining health and wellbeing, and the economy. The same applies to those who use social care services and the wider social care sector. There is a need to ensure a co-ordinated and effective response at all levels.
During the pandemic, the Better Care Support Team, Local Government Care and Health Improvement Programme and the Association of Directors of Adult Social Services devised a process for reviewing data and the issues facing particular local areas in response to COVID-19, and the Care Home Support Plan in particular. Through this approach, communication was issued about the implications of areas that experienced higher transmission of the disease to advise and assist authorities in their work with providers. This regional process could be strengthened by stronger input from local Health Protection Teams. There is also a need to ensure that there is a provider perspective in these discussions and review.
Spotlight: Single overview in the South East
For the last year, South East Association of Directors of Adult Social Services (ADASS) has supported a South East Health and Social Care Collaborative. This enables directors of adult social services and other system leaders to have a single, coherent 'offer' – an overview of the support and resources available to them collectively from regional and national organisations, including the LGA/CHIP programme, NHS Confederation and NHE England and Improvement, as well as South East ADASS. The Regional Chair of South East ADASS jointly chairs the steering group for the collaborative with NHE England and Improvement.
The South East has been able to build on the well-established work of the collaborative to integrate the new COVID-19 review process for care home support and resilience plans. Public Health England is now a key part of these regular weekly discussions. The benefits of this system-wide collaborative approach in the South East are:
-
detailed analysis of data sets including the Capacity Tracker, Public Health England reporting from pillar one and 2 testing and Joint Biosecurity Centre reporting
-
a highly informed and time-sensitive understanding of risk
-
direct and immediate DASS-to-DASS communication on issues arising which can be used to inform the Minister
-
targeted system support when required
-
informed on-going reporting by the Better Care Fund team
There is a need to ensure the adequate and co-ordinated representation of providers in the assurance process. Any model of representation needs to be agreed with the sector. There is a need to enable local associations and providers to be represented by a network of regional staff. This would ensure that whatever the key regional agenda – for example, the analysis of care home support plans, management of cluster local outbreaks, supply of PPE, application of mutual aid, roll-out of flu vaccinations – could be addressed by all of the relevant partners in an equal manner. Consideration would need to be given to the resource requirements.
This report recommends strengthening the sector response at a national level. It is also the case that any effective national approach needs a strong response from regional and local leaders who have the responsibility for the service and the local expertise and relationships.
Recommendation 37
Provider representation should be established in each area as part of the regional support to the sector and assurance for the sector. The model and arrangements need to be confirmed and implemented with the sector.
Action for: DHSC, Care Providers Alliance, with LGA and ADASS
Care Home Support Plan
The Care Home Support Plan was launched on 15 May 2020, alongside the provision of 13 indicators recorded on the Capacity Tracker - all 13 improved from between 12% and 48%, from 29 May to 10 August 2020.
The plan included a raft of important measures, based on the emerging international evidence, many of which were dependent on the importance of high quality working relationships between providers, local authorities, the health service and wider public services.
Underpinning this national framework have been efforts to promote close and effective working in the relationship between those commissioning services and providers in order to jointly meet the challenges posed by the virus.
Spotlight: Supporting care homes in Walsall
Walsall Council took a co-ordinated approach to supporting care homes, and established the Enhanced Quality in Care Team, which consists of social care staff, nursing, health visitors, GP, consultant, infection prevention control staff, pharmacist and the quality in care team. The Enhanced Quality in Care Team assesses care homes' risk level based on mortality rate, resident dependency, infection prevention and control measures implementation, use of PPE and staffing. It offers the homes hands-on tailored intervention to 'stabilise' them. The homes are given a plan for follow up with the quality in care team. Care homes have praised the support provided.
Spotlight: Provider hub in Hertfordshire
In March 2020, Hertfordshire County Council Adult Care Services in collaboration with the Hertfordshire Care Providers Association established a provider hub which brought together a 7-day phone helpline and email support for care providers to access. Support was provided across many issues including access to PPE, keyworker status and identity cards, staff capacity issues, infection prevention and control, clinical supplies, and accessing food and cleaning. The provider hub has helped guard against repetitive calls to providers and escalate any issues that cannot be resolved locally. Public health colleagues were engaged at an early stage ensuring that guidance, training and advice has been consistently available.
Options for restricting staff movement
There are several reasons for staff movement, including:
1) having a proportion of staff on zero-hours contracts enables flexibility in staff numbers for providers, including the ability to contract or expand the workforce in line with levels of occupancy
2) for some staff, the ability to choose shifts from different homes provides the ability to organise work around other responsibilities
3) the general shortage and movement of staff reflected in a 10% vacancy level and high turnover rates. This is, in part, likely to be due to the level of pay for the workforce
There is a national shortage of nurses across both health and social care. The terms and conditions in the health service are generally more favourable than those in social care.
National and international research has evidenced that a significant risk in outbreaks of COVID-19 in care homes is staff movement. The Vivaldi research (published 3 July 2020) demonstrated that homes were more than twice as likely to have had an outbreak if there was staff movement compared with homes where there was none. Identifying options to restrict staff movement is therefore a priority.
The research classified staff movement relating to:
a) bank staff (clinical such as nurses and care staff)
b) bank non-clinical
c) people who work elsewhere in addition to the care home
The Capacity Tracker data demonstrates that between 29 May 2020 and 20 July 2020, the percentage of homes that reported the ability to restrict staff movement increased from 78% to 92%.
Two workshops were held with the sector – a range of large, medium and small providers drawn from the profit and not-for-profit sector – to explore the issues in more detail and determine what further steps could be taken while maintaining essential services. The Local Government Association and the Association of Directors of Adult Social Services were also represented. We explored options, summarised below, with recommendations for next steps. However, more detailed work with providers has indicated that (pre-pandemic) most providers had between 7% and 10% of rostered hours carried out by staff who move between roles. More recently, this figure had reduced to between 0% and 3%.
Providers are concerned that this progress has been possible partly because partners of care workers were either furloughed or unemployed, enabling existing staff to work longer hours. While the economic impact on other sectors has enabled additional recruitment, the concern is that as economic activity picks up, the conditions that have led to high vacancy levels and 40% turnover of care staff (Skills for Care, 2019) will reapply. It is also the case that occupancy and demand has temporarily decreased. This has enabled providers to run a safe service with less vacancies on a temporary basis.
As part of the taskforce's work, the chair wrote to the sector emphasising the importance of restricting staff movement and paying full pay to staff who are isolating or absent through illness. Work also took place with the sector to support the development of an infrastructure including the national/regional/local arrangements for further delivery of the Care Home Support Plan.
Spotlight: Volunteers helping to fill workforce gaps in Leicester
Leicester City Council operates a 24/7 integrated crisis response service to facilitate hospital discharges and community step-up. If needed, this team can be redirected to support care homes as part of the council's emergency response service, in addition to the council's reablement service.
The local authority has developed a voluntary workforce scheme to support care homes, using volunteers sourced from both local authority staff and individuals from the voluntary and community sector. The scheme, which has been running since April 2020, gives capacity to ensure the safety of residents and minimises the movement of staff between establishments. This has helped where large-scale testing has meant that the identification of asymptomatic individuals may increase the numbers who need to self-isolate.
The scheme has filled gaps left where existing staff are sick or self-isolating by offering DBS-checked volunteers who have also undertaken the Skills for Care volunteer learning programmes and completed an induction programme. Several volunteers are currently working in the homes, with a number subsequently taking up full time employment as care workers.
Spotlight: Restricting staff movement in Wiltshire
Wiltshire Council, Wiltshire CCG, Wiltshire Health and Care and care home providers have collectively sought to restrict the movement of staff between care homes to reduce the spread of infection with any mutual aid being risk assessed. The majority of care homes have put in place robust contingency plans for staffing which have been shared with the council.
The COVID-19 team work with providers to identify their staffing needs and any mitigating actions that can be taken to reduce the impact. Where appropriate, provider business continuity plans are activated. Where additional staffing costs are incurred, additional COVID-19 costs claim forms can be submitted in line with the council's financial offer.
Where providers are unable to access sufficient staffing to meet their residents' needs, they inform the COVID-19 team. The COVID-19 team refer to the council operation's teams, Wiltshire Health and Care and the CCG to request staffing resources. A partnership agreement is put in place with the care home. To date, the council has provided 4 members of staff to a care home experiencing staffing shortages. The CCG has allocated 2 members of staff (nurses) for 3 months to support one home which has developed a hospital discharge support unit. The COVID-19 team will work with the provider to carry out business continuity planning, should the full requested resource not be available.
Cohorting and zoning to reduce risk of infection
The Association of Directors of Adult Social Services led a piece of work for the taskforce to identify appropriate levels of cohorting and zoning (isolating people within care homes who have tested positive for COVID-19 and the staff who support them and the facilities that are needed). This work has helped to enable local assessment of the safety and effectiveness, as well as suitability of particular care homes. The advice from this work is that following local assessment of the degree to which homes can meet cohorting and zoning best practice, local authorities will as necessary commission dedicated resources that enable safe care.
Spotlight: 'Pop-up' care home in Somerset
In partnership with Somerset Care Limited, the local authority opened up a new 37-bed 'pop-up' care home in Yeovil as an alternative accommodation for people who tested positive for COVID-19 or were displaying symptoms but could not safely return to their care home or own home. The scale and speed of the project was considerable, including a fit-out – that would usually take some up to 6 weeks – being achieved in just 2 days. At the start of the pandemic, the council issued an appeal for carers and received 184 applications. A total of 65 staff members were recruited, including a county councillor who retrained for the role. A registered manager for the home was redeployed via Somerset Clinical Commissioning Group.
Spotlight: Infection prevention preparedness tool launched in Newham
The London borough of Newham's commissioning, public health and safeguarding governance teams and its CCG have worked together to develop an infection prevention and control (IPC) preparedness tool. This allows the council and providers to identify when it is safe for them to receive residents being discharged from hospital. The tool considers the size and layout of the home, number of residents, how many have a high level of need, current IPC practice, and staffing capacity. Each home is reviewed on a regular basis using the tool to ensure their preparedness status is up-to-date, and that action is taken where necessary to increase safety.
Recommendation 38
Local authorities should review contingency arrangements for staffing shortages with the aim of reducing the need for staff movement.
Action for: Local authorities
Recommendation 39
In consultation with local government, central government should consider making regulations to give local authorities a responsibility for arranging a staff bank to help meet staffing shortages, where this is required. Arrangements should comply with good infection prevention control including weekly testing and infection prevention and control training.
Action for: DHSC
Recommendation 40
Further explore the level of exclusivity arrangements that exist with care agencies and how to increase them, reducing staff movement.
Action for: Providers
Recommendation 41
The cohorting and zoning recommendations developed by ADASS, working with providers and its implications for commissioning should be adopted across the country. This should include ensuring early partnership discussions with providers about the safety and feasibility of implementing these arrangements within their homes.
Action for: DHSC/ADASS and providers
Recommendation 42
Implement a national framework for learning reviews of care home outbreaks with subsequent advice on good practice and learning.
Action for: DHSC
Adult Social Care Action Plan
On 15 April 2020, the government published an Adult Social Care Action Plan with the intention of introducing measures aimed at:
-
controlling the spread of infection
-
supporting the workforce
-
supporting independence, supporting people at the end of their lives, and responding to individual needs
-
supporting local authorities and the providers of care
The taskforce carried out a review of the actions identified in the Adult Social Care Action Plan and the degree to which they had been delivered. Where they had not been fully delivered the review determined whether they were still relevant and covered elsewhere if required, for example in the taskforce recommendations.
Figure: Review of Adult Social Care Action Plan
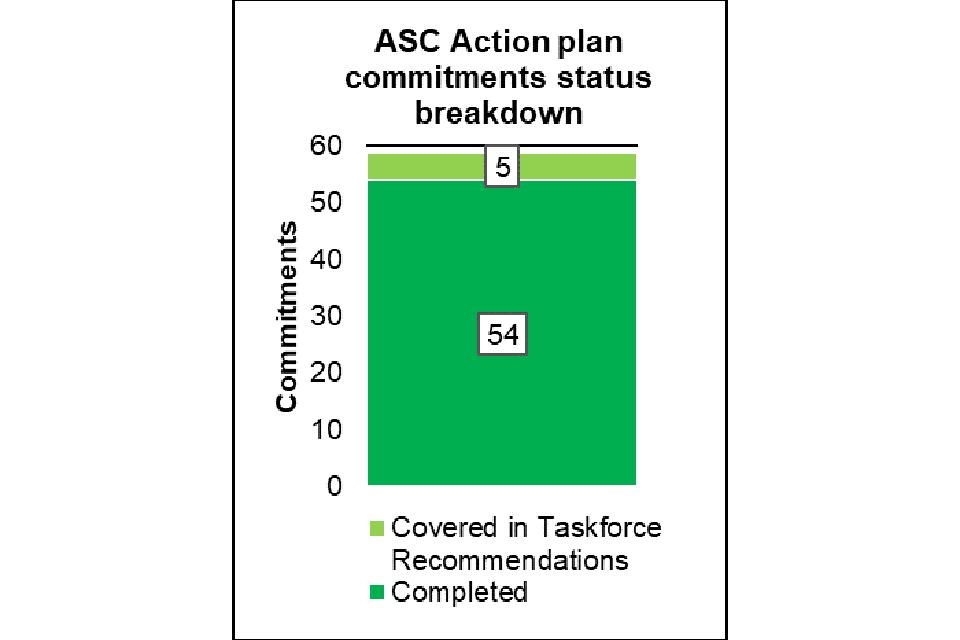
Out of 59 Adult Social Care Action Plan deliverable commitments, 54 have been completed.
This includes examples such as:
- 168.5 million items of PPE have been distributed to wholesalers and as an emergency drop 7 million straight to providers
- insight reports have been published with feedback from the sector on the current situation collected by the CQC
- local authorities have reported on how they have used the new funds with high compliance
- there are also many other complete actions under workforce, monitoring, wellbeing, testing and service user needs categories
There are another 5 commitments that are ongoing and linked to the taskforce recommendations.
The conclusion from this review
The majority of the action plan has been completed with remaining parts being covered in the taskforce recommendations
Almost all deliverable commitments of the Adult Social Care Action Plan have been completed with only a few remaining. All of these are covered by the taskforce recommendations and include areas such as helping providers' cashflow by making payments in advance, supporting unpaid carers and redeployment of nursing staff.
Several elements of the action plan will also be covered in the government's proposed winter plan
There are some time-bound elements to the plan that have been delivered and require no further action, but there are also parts that require further consideration going forward. These are taken forward by the winter plan, taking into account the changing environment and learnings that have come through the regional response loop, stakeholder feedback or otherwise.
The taskforce also carried out a review of completed actions against the World Health Organisation report, Preventing and managing COVID-19 across long-term care services, and have included any outstanding recommendations.
Development of a digital tool as part of a new information dashboard could give a view of implementation measures at a national, regional and local level
The proposal is to use data (both from the Capacity Tracker for care homes and from the CQC domiciliary care survey) to show how well some of these specific measures are being implemented across the country, highlighting local variation and areas where further support is required and showing trends over time. This information further enhances the regional response loop work led by the Better Care Fund team.
BAME communities and inequalities
In line with the advice of the BAME Advisory Group there is an overall need to strengthen application of consideration of the needs of service users, carers and the workforce from BAME communities and there is evidence that this is being carried out. It is therefore recommended that further advice is provided and that local authorities take the necessary steps to address inequalities.
Safeguarding
The pandemic places particular challenges in ensuring that potential safeguarding issues are prevented where possible, known and acted upon. The evidence is that isolation can increase the risks. This emphasises the importance of ensuring that local authorities can continue to exercise their statutory responsibilities with local safeguarding boards, that CQC have been able to recommence inspections and that (for example) visiting arrangements are safely enabled wherever possible.
Recommendation 43
In implementing the taskforce Action Plan, local authorities should ensure they take steps, in line with the public sector equality duty of the Equalities Act 2010, to ensure they evidence and address the inequality of outcomes for people affected by COVID-19. DHSC should make available further specific advice for the sector in addressing inequalities.
Action for: DHSC / local authorities
Homecare and other community care settings
In view of the level of outbreaks and the evidence of risk there has inevitably been a focus on care homes. The opportunity of the taskforce was to look widely across the sector to consider other areas. Responding to COVID-19 requires innovative approaches enabling safe ways for service users and carers to be supported. This involves supporting informal as well as formal care arrangements, for example, the shielding bubbles involving people with disabilities or long-term care needs is an essential part of having a broader network of support. The advisory groups emphasised the importance of this in making sure that people are connected and that it is not entirely dependent upon the direct intervention of statutory services.
In addition to general guidance about managing the safety of groups of people at risk, there is also a need for assessment and support for people to balance their safety from COVID-19 with access to support and services and more generally supporting overall health and wellbeing. In each situation there is a balance of risk to be navigated.
Flexibility within the framework of national advice applied to individuals and families is an essential part of person-centred, co-ordinated care. People with lived experience of services consistently refer to the need to have as much control as possible over decision- making, relationships, information and the resources – even though capacity varies. The Self-directed Support Advisory Group cited the importance of flexibility in the use of personal budgets in the pandemic given that people are faced with extraordinary circumstances.
Finding innovative ways to provide outreach virtual contact, short breaks and wider support is critical. In many places there is evidence of such innovative approaches – these need to be applied right across the country. Given the crucial role of informal carers, whose numbers have increased significantly during COVID-19, there is a strong case for seeing informal carers as key workers. We heard of the importance of people knowing who to contact as well as a proactive review of people's needs. In addition, the Mental Health Advisory Group highlighted the importance of continued investment in advocacy for those people who need such support to access appropriate services. The issues arising for testing for care staff outside care homes have been included in the recommendations in the section on Testing.
The TSA Sector Insight Report (July 2020) includes a number of innovative examples of care from a range of care settings across the country, including best practice case studies in Hampshire and Stockport, which demonstrate the capabilities of protecting people and keeping them connected.
Day services
The Carers Advisory Group, some local authorities and voluntary organisations have highlighted the challenge of opening up day services. Guidance has been published on the Social Care Institute for Excellence (SCIE) website but the requirements of social distancing mean that there is less capacity for day services than normal and safe transport also limits the number who can travel.
The advisory group emphasised the challenge for carers of all ages. For example, they have emphasised the need to recognise the responsibilities of young carers and the importance of them having the ability to return to school while being reassured of the safety and wellbeing of their parents. This shows the importance of opening up day services or finding alternative solutions.
Recommendation 44
A mechanism should be developed for sharing good practice on support for young carers to engage effectively with education providers.
Action for: DHSC
Some work was undertaken by the DHSC and the taskforce to understand in more detail the position. There is evidence of considerable creativity being used to deliver alternatives. This is a particularly important provision, not only for service users, but also many carers who depend upon this support for respite and to help support carers to work. Where normal services cannot be resumed in full, local authorities should explore alternative care options to enable people to return to work where possible.
Spotlight: Day services in Derbyshire
The difficult decision to shut all day services across Derbyshire was taken in March 2020 at the onset of the national lockdown. The solution developed was to open several rooms within a centrally located in-house day service building, on a sessional basis. People were prioritised who services knew to be at particular risk of a serious decline in their mental health. Each room offered different activities such as music therapy, gardening, dancing, art and crafts, available for people with complex support needs. Prior to accessing the service, individual risk assessments were undertaken, protocols developed to ensure compliance with public health guidance regarding infection control, and staff and service users had access to the full range of PPE. Staff from across Derbyshire volunteered to work at the centre, some needed extra training and support. By working collaboratively across departments, solutions were found to barriers such as transport and training, for example, the local autism advice service delivered training via their YouTube channel.
Recommendation 45
The government, in conjunction with local government, carers and service users should establish a project to ensure that day service provision is opened up across the country and the innovative examples of alternatives are spread nationwide.
Action for: DHSC / ADASS / providers
Home care
A workshop was held to consider the evidence of the need for support in the home care sector. The sector has a similar number of staff (more than 600,000) to the care home sector but provides care for many more people. The workshop highlighted the need to ensure there is ringfenced money for community care in the event that the Infection Control Fund is continued. The case for this is that for effective and appropriate infection prevention, community care staff would need to be paid full wages while sick, with backfill arrangements in place.
A range of issues were considered and these are listed below:
-
PPE
-
testing
-
flu vaccination
-
shielding
-
training
-
occupational health
-
cohorting
-
clinical support
-
self-paying market
-
personal assistants and direct employees
-
winter and second wave guidance
-
other opportunities
The issues picked up from this workshop are either covered in other recommendations in this report or have been added below. Discussions were wide-ranging and included an emphasis on the importance of a free and accessible process for care staff to ensure the maximum take-up of the vaccination. The workshop found that guidance is required on how and when to come out of shielding. The workshop heard calls for greater access to training on infection prevention and control in care homes and greater access to occupational health services (existing access is mainly through a phone service). There is particular concern about the access of occupational health services to small providers. It is an employer's responsibility to make access to such schemes a feature of their offer to staff. However, in the current circumstances it is appropriate to ask government to explore whether it is possible to provide a framework from which employers can access and pay for the support.
It was mentioned that some are currently not entirely clear whether cohorting has been done before and whether it works for domiciliary care. The sector asked if some priority could be given to the support of users of social care services (based on need) as this group is likely to be among those with greatest need who have previously been asked to 'shield'. It was stated that there is a need to ensure the winter plan and any second wave guidance include community care. The workshop heard there is a risk on provider liability – emphasising the importance of good working relationships between provider and commissioners at a local level and effective winter planning. A question was also asked at the workshop, stating that as there is currently more capacity in the system than historically, could we explore how this could be used to improve the service, for example by supporting hospital discharge?
Recommendation 46
Government and local authorities should review the options to make occupational health services available to the sector where there are gaps.
Action for: DHSC / LGA
Managing community outbreaks and the response of social care
The taskforce chair attended weekly meetings of the Joint Biosecurity (JBC) Local Action Committee (Gold), chaired by the Secretary of State. The temporary Director for testing in social care (former Chief Nursing Officer for England) attended the silver committee, chaired by the Chief Medical Officer. The following were put in place:
-
arrangements for follow-up once areas of the country of highest risk due to rates of transmission have been considered by JBC
-
arrangements for follow-up are through the Local Government Care and Health Improvement Team
-
recommendations, as appropriate, to local directors of adult social services, directors of public health, accountable officers, providers, and directors of nursing in clinical commissioning groups
The taskforce worked with NHS Test and Trace to identify arrangements to ensure that social care is a priority in the management of local outbreaks, with round tables and webinars to inform the sector about the issues and actions that have been required in the early work in managing community outbreaks, and the actions that need to ensue in the event of a local outbreak. The actions include:
-
good communication locally with the sector on emerging risk
-
reinforcing guidance on infection prevention and control and social distancing, including between staff in common areas
-
prioritising testing to those services of greatest risk
-
regular contact with care homes and other social care services on infection control, risk assessment, outbreaks, staffing, test results and PPE supply
-
assuring clinical lead arrangements in primary care for care homes and their residents
-
consideration of changing visiting arrangements and ensure that all individuals who visit to provide services conform to infection prevention and control standards
-
reviewing high risk factors (for example, reducing/eliminating staff movement, paying full pay for sickness/absence, and social distancing outside work)
-
risk summits – review of higher risk settings
The taskforce worked with NHS Test and Trace to arrange a workshop with the following objectives:
-
build a mutual understanding of the roles and responsibilities between JBC, Test and Trace and Contain, and social care
-
identify the data flows, processes and actions in the event of higher infection rates in local communities and in social care
-
formulate the outcomes into written joint protocols and operating procedure between JBC and social care
This work aligns with the recommendation of the Guidance, Good Practice and Innovation Advisory Group which advised that there should be new guidance for commissioners, providers and others in relation to local outbreaks.
The outcomes of the workshop were to confirm that the existing advice and to provide further advice on the following areas:
-
data – the need to provide more data on testing, incidence, outbreaks, Care Homes Support Plan, infection, prevention and control measures and CQC ratings in one place, in an accessible way to the system. This work is underway as part of the development of a national dashboard. The next steps are to ensure that the necessary arrangements are in place for sharing the data and ensuring it is presented in a way that national and local organisations, including providers, can access and use to inform their actions
-
local initiation – ensuring improved local access to data (as above) and guidance outside of the JBC/Contain framework so they can self-identify changes in risk. There is a recognition that systems are already doing this with the data they have and a need to understand how the wider system can support
-
provider representation – consideration to be given of formalising the role of regional and national provider representatives, encouraging local provider representation arrangements
-
breadth of support – the care homes work is well developed. Support needs to be reviewed for informal care settings, domiciliary care, and extra care/supported living
-
advice, guidance and communications – documentation around this needs to be finalised and communicated. There is an emphasis on the importance of system leadership and collaboration with a line of sight to inform national interventions
-
there is a need to provide appropriate information and advice to carers including using the recovery plan for carers developed by Carers UK
-
the guidance should reflect the balance between standardisation and allowing the need for local risk management and decision making. For example, it was advised that visitor guidance should remain flexible and proportionate to risk levels and circumstances, balancing different risks
-
there is a need to develop simple flow charts for different organisations so that it is easy to follow an individual role; develop communication templates and for local authorities to review the communication channels for all care providers (including non-registered) in advance of a local outbreak (where not already developed)
Recommendation 47
The actions identified in the workshop should be implemented in September 2020.
Action for: DHSC / NHS Test and Trace
Recommendation 48
NHS Test and Trace to ensure that local authorities (DASSs and DPHs) have timely access to test results from residents and staff in care settings, to enable them to manage, effectively, the risk of incidents or outbreaks.
Action: DHSC / NHS Test and Trace
Recommendation 49
There should be a monthly review of the specific arrangements and protocols between NHS Test and Trace, its Contain function, and social care. This is to ensure consistency of approach as well as providing appropriate and proportionate support to localities and the sector.
Action for: DHSC / NHS Test and Trace
Recommendation 50
NHS Test and Trace should determine whether those tested positive for COVID-19 (or their contacts) are working in the care sector, or are unpaid carers, to enable the appropriate advice and support to be offered.
Action for: DHSC / NHS Test and Trace
Key themes emerging from the taskforce advisory groups
As previously highlighted, 8 subject-specific advisory groups have fed into this main report, having worked at speed and with great dedication to produce their findings. We do not intend to repeat all that the advisory groups have said in their individual, detailed and comprehensive reports. The 8 individual advisory group reports are published alongside this main document as appendices – each report demonstrates the considerable expertise and insight of its members.
The advisory groups drew their expertise from various organisations and leaders in the sector, including through the lens of those who have most experience of what works, people with lived experience of social care. The reports should all be read and seen as a natural extension of this main report. The reports cover a range of issues and make some specific recommendations and otherwise provide more general advice about the approach and how things should be done. This advice and insight have been used to inform and, in some cases, bolster the analysis and recommendations in the overall report. The groups were all supported by DHSC policy leads and we advise that further work is undertaken to respond to and determine how to enact the advice given. Some key points and themes that have emerged from the taskforce advisory groups include:
-
ensuring that our future plans, for this winter and beyond, take into account the specific needs of those with protected characteristics or who may be disadvantaged in society in some way
-
better understanding the disproportionate impact of COVID-19 on BAME people and the differences within ethnic groups, providing more support for BAME frontline workers, and ensuring equity of care across all population groups
-
making future planning for the social care sector inclusive and accessible
-
ensuring that communications, local and national, are conveyed in a way that are accessible to everyone in all communities, with culturally appropriate messages
-
reviewing which groups receive priority for testing and/or vaccines to include carers, for example, and giving unpaid carers a similar status to key workers
-
maximising digital and tech opportunities across local government, health, the voluntary sector and for public, patients and carers (while being aware of the dangers of digital exclusion)
-
improving data collection and analysis in the care sector (for example, on COVID-19 deaths for people with a learning disability and/or autism) and making better use of available data
-
learning from best practice in the response to the pandemic and supporting other health and care communities to rapidly adopt from those who can demonstrate success
-
making all the necessary steps to ensure sustainability of the care sector, supporting both recruitment and retention in varied job roles across the sector, investing in the confidence and capability of this workforce, and considering how best to manage situations where provider organisations are at risk of collapse
-
embedding the practice of co-production (including with staff, individuals with lived experience and carers) into all COVID-19 planning both locally and nationally
-
being aware of the importance of maintaining existing health and care services and other sources of support as much as possible throughout the pandemic and beyond, in order to combat loneliness and enhance health, wellbeing and work
-
promoting parity of esteem between mental health and physical health, and between health and social care
-
getting on the front foot with our care responsibilities, not just waiting to learn of people in difficulty but proactively seeking and supporting individuals, and connecting communities
-
rapidly reviewing existing guidance and ensuring that future guidance, for example on local lockdowns, is clear and understandable to all local authorities, statutory agencies and to all communities
-
commissioning a rapid evidence review to understand why older people and people with dementia are at such high risk from COVID-19 and how best they should be cared for and treated
-
ensuring effective safeguarding, including restoring visiting to care homes and services into people's homes, will help mitigate these risks
-
kick-starting some of the longer-term changes by investing in some urgent infrastructure elements around occupational health, recruitment, retention and pay, in order for us to have a COVID-19-ready workforce
Recommendation 51
The advice and recommendations of the advisory groups should be considered by the DHSC and a response be provided on the advice and recommendations and how they are to be taken forward.
Action for: DHSC
Planning for the next phase of the pandemic
This report sets out the progress and learning from the first phase of the pandemic in informing advice and recommendations to government and the social care sector. Many of the recommendations should be picked up in the government's planned national winter plan. In order for the sector to be as resilient as possible, all local authorities and all providers need to formulate their own plans in line with the national winter plan.
The 3 key elements to this are:
-
the national offer – key responsibilities of government are assuring the provision of personal protective equipment (PPE); a national testing strategy for social care, continuously reviewed in line with best international evidence; and resources, ensuring that the extra costs associated with the pandemic by local authorities and providers can be met by government. In addition, we need to ensure there is an effective, planned relationship between adult social care and the NHS
-
regional – agencies that work at a regional level need to ensure they have mechanisms in place and plans that assure the effectiveness, capability and risk mitigation in local systems
-
local – local authorities, with partners and providers, have had a particularly challenging task in responding to the challenges of the pandemic alongside their usual responsibilities. The next phase requires all agencies to work together and put in place plans to protect and connect service users and carers in accordance with the national winter plan and best practice. The challenge of COVID-19 is the need to ensure that people receive access to health and social care services and maintain their safety and wellbeing. This will require health and care services locally to work hand in glove to meet the needs of their population throughout the next phase. Sustainability and transformation partnerships and integrated care systems have a key role in supporting the plans and response at a local level
Many places will already have plans but it is our advice that these should be reviewed and refreshed and transparently available to ensure resilience and give confidence to the public.
Recommendation 52
Following the publication of the national winter plan, each local authority and provider should have in place its own winter plan to build resilience and give confidence to the public. This should include business continuity planning for organisations and contingency planning for service users and carers in situations where there are complex arrangements which depend upon a few key individuals and family carers.
Action for: DHSC with local authorities and providers
References
-
Office for National Statistics: Impact of coronavirus in care homes in England: 26 May to 19 June 2020 ↩
