Government response: Health is everyone’s business
Updated 4 October 2021
Government response to the consultation on proposals to reduce ill-health related job loss
Presented to Parliament by the Secretary of State for Work and Pensions on behalf of the Department for Work and Pensions and the Department of Health and Social Care by Command of Her Majesty.
© Crown copyright 2021
This publication is licensed under the terms of the Open Government Licence v3.0 except where otherwise stated. To view this licence, visit The National Archives.
Where we have identified any third party copyright information you will need to obtain permission from the copyright holders concerned.
This publication is available at www.gov.uk/official-documents.
Any enquiries regarding this publication should be sent to us at workandhealthunit.consultationteam@dwp.gov.uk
ISBN 978-1-5286-2363-6
CCS1120523008
CP 509
July 2021
Correction slip
Title
Health is everyone’s business
Government response to the consultation on proposals to reduce ill health related job loss
Session: 2021/2022
CP 509
ISBN: 978 -1-5286-2363-6
Correction
Text currently reads:
P.30 “Research conducted by the Society of Occupational Medicine (SOM) during the early stages of the crisis showed over three quarters of NHS OH providers and more than half of in-house OH providers said their workloads had increased.47”
P.32 – “A survey by the Society of Occupational Medicine (SOM) conducted in April 2020 showed three quarters of practitioners were spending an increased amount of time providing remote consultations”
Text should read:
P.30 “Research conducted by The At Work Partnership during the early stages of the crisis showed over three quarters of NHS OH providers and more than half of in-house OH providers said their workloads had increased.”
P.32 – “A survey by The At Work Partnership conducted in April 2020 showed three quarters of practitioners were spending an increased amount of time providing remote consultations”
Date of correction: 23 September 2021
Ministerial foreword
We are living and working longer than ever before. Being in work can help raise living standards, move people out of poverty and help reduce health inequalities. This not only benefits individuals and employers, through workforce retention, but also wider society, supporting our commitment to level up the country and enabling us to build back better.
The measures outlined in this response are designed to minimise the risk of ill-health related job loss through providing employers with access to good quality information and advice, supporting employers and employees during sickness absence, enabling Small and Medium Enterprises (SMEs) to reap the benefits of Occupational Health (OH), and proposals to enable better use of the fit note. This is just one part of our approach to supporting disabled people and those with long-term health conditions. The ‘Health and Disability Support Green Paper’[footnote 1] led by DWP considers improvements to health and disability benefits in the short to medium term whilst also starting a discussion about more fundamental changes. Together these build on the commitments we made in ‘Improving Lives: the future of work, health and disability’,[footnote 2] including our ambition to see one million more disabled people in work by 2027. In addition, they complement the National Disability Strategy which sets out practical changes to improve disabled people’s everyday lives, helping to achieve equity of opportunities so that everyone can fully participate in the life of this country.
Disabled people and those with long-term health conditions remain under-represented in the labour market and there is significant variation in how employers manage work and health.[footnote 3] Before COVID-19, an estimated 300,000 disabled people fell out of work every year.[footnote 4] Society is missing out on their valuable contribution to the workforce, whilst individuals themselves are missing out on the health and financial benefits associated with good quality work.
While COVID-19 has brought significant economic challenges, with necessary economic restrictions leading to higher rates of redundancy and unemployment, we have also seen many employers harness the power of technology and introduce greater flexibility in the way work is done. Many employers have gone above and beyond in helping their employees juggle caring responsibilities, work flexibly and work from home throughout the pandemic.[footnote 5][footnote 6][footnote 7]
As the UK continues to recover and comes to better understand the longer-term impacts of COVID-19, it is more important than ever that disabled people and those with long-term health conditions are supported to remain in work so that no group is left behind. This government is committed to building back better, and providing the right support to disabled people and people with long-term health conditions will help create a healthier population with a higher level of employment that benefits productivity and drives the economy.
By working together to look after the health and prosperity of our people and our businesses, we champion not only the wellbeing of every individual in this country but also the nation as a whole.
Justin Tomlinson MP
Minister for Disabled People, Health and Work
Jo Churchill MP
Minister for Prevention, Public Health and Primary Care
Executive summary
In November 2017, we published ‘Improving Lives: The Future of Work, Health and Disability’[footnote 8] which set out our plans to transform the employment prospects for disabled people and those with long-term health conditions over the next 10 years. In it, government set a goal to see a million more disabled people in work by 2027 and to realise an ambitious vision for society where ‘people understand and act positively upon the important relationship between health, work and disability’. Government continues to focus efforts across three key settings in order to achieve this: the welfare system, the workplace and the healthcare system.
‘Health is everyone’s business’ put forward a number of proposals to minimise the risk of ill-health related job loss through better workplace support for disabled people and those with long-term health conditions. It explored changes to Statutory Sick Pay, Occupational Health, information and advice, and employer guidance. The Health and Disability Support Green Paper[footnote 9] explores how to improve support for disabled people through the welfare system. Together, with the forthcoming National Disability Strategy, they are part of this government’s holistic approach to support disabled people and those with long-term health conditions to live full and independent lives.
Whilst this response focuses on the measures outlined in ‘Health is everyone’s business’, work beyond the scope of this response has continued at pace. For example, we have taken steps, along with local partners, to advance the work and health agenda, in particular in the area of prevention. We also want to ensure there is better integration between health and employment support services which will help people with long-term health conditions to enter and stay in work.
The majority of employers agree that there is a link between work and the health of their employees.[footnote 10] Employers who invest in the health and wellbeing of their workforce benefit from reduced sickness absence, increased productivity and improved workplace retention. Employees benefit from a supportive environment in which they can thrive and perform at their best. Being in work can help someone to be independent in the widest sense: by having purpose and self-esteem, by building relationships and by being financially independent.
As ‘Improving Lives’ set out, we want to see individuals, where appropriate, benefit from a preventative approach to ill-health and an environment which supports health promotion. We want to see employers creating healthier workplaces and offering the right support to their staff. We also want both employers and their staff to be supported by a health system which promotes good health and helps them to better manage their conditions. Much of the focus of this document is on the role employers themselves play, but we also recognise that when individual employees are struggling with health issues and engaging with the health system, there are opportunities to provide them with advice to help them manage the employment impact of their condition. To that end, we have:
- integrated Employment Advice provision in the NHS’s Improving Access to Psychological Therapy (IAPT) services in England[footnote 11]
- invested in Individual Placement and Support (IPS) with local partners, to test new ways of supporting people to enter, re-enter and stay in work
We have also worked with NHS England/Improvement and Public Health England to explore barriers and enablers to partnership working on work and health in local systems. We are currently undertaking further exploratory work on the development of partnerships, strategies and greater integration of services at a local level.
Impact of COVID-19
The consultation was published at a time when employment was at a near historic high and disabled people’s employment had also improved significantly; between October to December 2013 and October to December 2019, the number of working age disabled people in employment increased by 1.4m, from 3.0m to 4.4m.[footnote 12] It set out to build on that progress by introducing a comprehensive and balanced package of measures to support more disabled people and people with long-term health conditions to remain in work.[footnote 13] Since then, the impact of the COVID-19 pandemic has been widely felt across the economy and society.
In response to the pandemic, government acted swiftly to protect the incomes of millions of people including through the Coronavirus Job Retention Scheme (CJRS) and Self-Employed Income Support Scheme (SEISS).[footnote 14] This was followed by the Chancellor’s Plan for Jobs which set out to protect, support and create jobs. At Budget 2021, government announced the extension of the CJRS and SEISS alongside an additional £5bn for new Restart Grants and a new UK-wide Recovery Loan Scheme which will make available loans to help businesses of all sizes through the next stage of recovery. This combined economic response is one of the most comprehensive and generous in the world.
The pandemic also highlighted the important role that health professionals play in the work and health agenda. OH professionals, who provide expert advice and support on work and health issues, have played a critical role in supporting the response to COVID-19. For example, they have supported employers to provide advice on workplace adjustments, and supported individuals recovering from COVID-19 to return to work. Finally, we have taken a cross-government approach to considering and responding to the challenges to mental health and wellbeing presented by the pandemic, contributing to the COVID-19 Mental Health and Wellbeing Recovery Action Plan which was published 27 March 2021.[footnote 15] This is the government’s plan to prevent, mitigate and respond to the mental health impacts of the pandemic during 2021 and 2022.
The impact of the pandemic, including on the labour market and health of the nation, increases the need to progress the important shared agenda of work and health. The package of measures announced here reflects feedback from the consultation, while acknowledging the impact of COVID-19.
This balanced package of measures will enable and encourage employers to take greater responsibility for the health and wellbeing of their employees, by offering increased government support including through improved information and advice and access to OH provision.
Chapter 1 sets out how government will provide employers with access to good quality information and advice. Employers, and small and medium sized enterprises (SMEs) in particular, may lack the time, capacity or expertise to manage health events in the workplace, or to search for the most relevant guidance. Employers have told us that while they trust government advice in this area, the current information on offer is fragmented and not always easy to apply to real-world problems.
Respondents asked for better integrated advice and information that is easier to find and act upon. Government has improved guidance for employers and employees in response to the pandemic – including, on returning to workplaces safely. Government now intends to build on this by refining the information and advice given to employers on health, work and disability. This will be easy to navigate and readily usable, especially for SMEs.
Chapter 2 outlines government plans to support employers and employees during sickness absence. The majority of respondents agreed that statutory guidance should be strengthened, stating that clear guidelines would give employers more confidence to act and provide consistency in their approach. Government has therefore asked the Health and Safety Executive (HSE) to work with other arm’s length bodies (ALBs) to develop non-statutory guidance to support disabled people and people with long-term health conditions to remain in work, and on managing any related sickness absence. HSE will also explore introducing statutory guidance in this area.
Although respondents supported the intent of the proposal, there was concern that introducing a new right would risk undermining existing workplace protections, most notably the duty to make reasonable adjustments. In particular In light of feedback government has decided not to proceed with the consultation proposal to introduce a new ‘right to request work(place) modifications’ on health grounds but will instead take steps to increase awareness and understanding of existing workplace rights and responsibilities, in particular the duty to make reasonable adjustments under the Equality Act 2010, we heard concerns that a right to request workplace modifications may legitimise refusing requests for adjustments and detract from the positive duty on employers to make reasonable adjustments.
Chapter three covers Statutory Sick Pay (SSP). The consultation sought views on a range of measures related to Statutory Sick Pay. These measures sought to make the system more flexible, simple, and responsive. The pandemic has shone a light on the importance of SSP and over the last year government has made several changes to the system to support those who were self-isolating and unable to work as a result of COVID-19.
Government maintains that the pandemic was not the right time to introduce changes to the rate of SSP or its eligibility criteria. This would have placed an immediate and direct cost on employers at a time where most were struggling and could have put more jobs at risk. Government instead prioritised changes which could provide immediate financial support to individuals, including changes to the wider welfare system, the introduction of the Test and Trace Support Payment and wider economic support such as the Coronavirus Jobs Retention Scheme.
As we emerge from the pandemic, there is space to take a broader look at the role of SSP. Chapter three covers the feedback from respondents to the proposals in the consultation that covered SSP.
Chapter 4 outlines the steps that government is taking to enable SMEs and self-employed people to reap the benefits of expert health and work support including OH. This will be informed by learning from the innovations that have underpinned the health system’s response to the pandemic, with some evidence of increased demand for OH as more individuals adapt to new working environments and require support to return to work. The uptake of other measures outlined in this package is also likely to increase demand for OH. Small employers are five times less likely to invest in OH services than large employers.[footnote 16] Government will seek to address this by testing and evaluating the impact of a subsidy for SMEs and the self-employed, designed to reduce the cost of accessing suitable OH. The evidence and affordability of a subsidy, alongside developments in OH reform policies, will inform the case for a potential fixed term roll-out in the future.
More accessible OH services may lead to a rise in demand, and potential new customers of OH will require support to ensure they are not purchasing inappropriate or low-value services. Government will take action to improve information and guidance on purchasing OH and explore the potential of outcome-linked measures to support providers to improve and innovate, helping employers to choose the most appropriate services for their needs. This includes piloting outcome-linked metrics with OH providers and employers which could be used to support continual provider improvement and improve employer choice.
Government will work with the market to explore how it can support faster innovation in OH particularly in relation to innovative ideas that prioritise new OH service models and make greater use of technology, with the aim of increasing SME/self-employed purchasing of OH. Government is also committed to working with key delivery partners to explore the potential merits of a new Centre for Work and Health Research that could strengthen the research infrastructure that supports long-term innovation in OH.
The chapter concludes by addressing concerns over shortages in the OH workforce and details government plans to respond by considering methods to promote the expansion of clinical roles, improving OH multidisciplinary workforce models which capture both clinical and non-clinical roles, developing new training approaches and establishing an OH leadership function to help drive the OH workforce strategy.
Chapter 5 sets out other issues raised during the consultation which include insurance, tax, Access to Work and proposals to enable better use of the fit note, a key tool which can be used to support workplace conversations and returns to work. Although not in the consultation, many respondents took the opportunity to share views about how the fit note process could be improved. There was a general consensus that the fit note remains an important tool but should be reformed so that it better supports people to stay in and return to work. The launch of the Isolation Note in response to COVID-19 has demonstrated the flexibility and responsiveness of employers and the healthcare system through their acceptance and use of an alternative form of evidence. Government intends to build on this learning and continue to explore opportunities for digital transformation of medical evidence provision. Government is also exploring extending fit note certification to a wider group of healthcare professionals and introducing digital certifying of fit notes as well as looking towards further opportunities to make the fit note interactive. These changes will make the fit note a more effective tool in supporting healthcare professionals to deliver holistic health and work conversations that the government believes are essential in supporting their patients to remain in, or return to, work.
Some respondents highlighted the importance of insurance products as another way of supporting workers’ health and wellbeing. Government welcomes recent proposals from the industry body Group Risk Development (GRiD) to develop a ‘consensus statement’ which aims to enhance employer guidance, improve employers’ awareness of the link between good work and good health, and promote the use of expert-led support services. Government will continue to work with the industry to improve awareness among employers and self-employed people of the benefits that protection policies can provide.
Several larger organisations called for tax incentives. In response to early consultation feedback and to recognise the variable availability of welfare counselling, changes were made in the March 2020 Budget to enable employers to provide non-taxable counselling services. This includes related medical treatment, such as cognitive behavioural therapy. The changes took effect from April 2020.
A number of respondents commented on the valuable contribution Access to Work makes in supporting disabled people and those with long-term health conditions to receive adjustments to enter into and remain in employment, and told us they thought more could be done to promote the service among employers and individuals. Government continues to promote Access to Work as part of Disability Confident and is undertaking further marketing and promotion of the Access to Work programme.
An overview of the potential costs and benefits of the full policy package set out in this response is given in the Annex, along with the methodology of measuring these impacts.[footnote 17] It supports a balanced package of measures in which both government and employers go further to support health and wellbeing at – and through – work. It describes the costs and benefits to business, and the wider societal benefits the measures will bring.
Introduction
‘Health is everyone’s business’ set out a number of proposals to minimise the risk of ill-health related job loss. Prior to COVID-19, there were around 12.7m working-age people with a long-term health condition, including 7.6m disabled people whose condition reduces their ability to carry out day to day activities.[footnote 18] Over the course of a year, around 1.4m working-age people had at least one sickness absence lasting four weeks or longer.[footnote 19] The likelihood of a return to work reduces the longer the individual experiences sickness absence.[footnote 20] Disabled people were 10 times more likely to have a spell of long-term sickness absence (LTSA) and leave work following it than non-disabled people.[footnote 21] The research is clear. Early and sustained support by employers, including workplace adjustments, is an effective way to minimise the risk of ill-health related job loss. Employers agree there is a strong link between work and health; however, there is significant variation in the level of support offered by employers.[footnote 22][footnote 23] Those who have experienced incidences of disability or long-term sickness absence in their workforce are more likely to have support mechanisms in place; larger employers are more likely to have dedicated HR support as well as access to formal health and wellbeing services such as OH.
The Chancellor announced the Plan for Jobs 2020 as the second phase of the UK’s recovery from the pandemic. The plan builds on the £160 billion support package provided in the first phase by supporting, creating and protecting jobs across the UK. As well as supporting those who have lost their jobs, we need to continue to improve retention. COVID-19 has made the consultation’s aim of minimising the risk of ill-health related job loss even more important, as the UK continues to recover. Before the start of the pandemic, the general trend in disability employment had been positive since 2014, when comparable records began. The pandemic initially reversed these trends with the disability employment rate falling and the disability employment gap widening during the middle of 2020. The employment rates, for both disabled and non-disabled people are still below their pre-pandemic levels but the disability employment gap narrowed in late 2020/early 2021. For example, in the 12 months to March 2021 the disability employment rate decreased by 1.2 percentage points but the disability employment gap decreased by 0.2 percentage points. This suggests that the disability employment rate is not currently being disproportionately impacted by the pandemic.[footnote 24] Emerging evidence suggests that there has been a deterioration in people’s mental health, particularly disabled people’s mental health.[footnote 25] In addition, over half of those facing redundancy due to COVID-19 are either disabled or have a long-term health condition.[footnote 26] More widely, increased productivity through a healthier workforce supports the economic recovery whilst a healthier population also reduces pressure on both the health and welfare systems.
The measures government is taking forward provide greater clarity around employer/employee rights and responsibilities; recognise the important role of OH; and reinforce the need for employers to have access to clear and compelling information and advice that is easy to understand, authoritative and accessible.
These measures support the government’s ambition to see one million more disabled people in work by 2027 and build on commitments made in ‘Improving Lives: The Future of Work, Health and Disability’.[footnote 27] This work will also complement the Health and Disability Support Green Paper, which focuses on improving employment support and enabling independent living, and the National Disability Strategy which will address broader issues which can unfairly limit opportunities for disabled people, alongside recent action announced by government to tackle obesity and help people live healthier lives.
The challenge cannot be solved easily or quickly, but by working with employers and healthcare professionals together we can start building a system that better supports disabled people and those with long-term health conditions to remain in work.
This document forms the government’s response to the ‘Health is everyone’s business’ consultation. It provides an overview of the responses received and provides details of what government intends to do next to take forward the package of measures.
How we consulted
The government launched the consultation ‘Health is everyone’s business’ on 15 July 2019. The consultation closed on 7 October 2019. The consultation was hosted online, accessible via GOV.UK. In total, 485 responses were submitted electronically. Table 1 shows a breakdown by respondent type. The majority of responses came from individuals and employers (or their representatives), followed by charities, healthcare professionals and trade unions.
Table 1: Responses to ‘Health is everyone’s business’ by respondent type
| Respondent Type | Responses | % |
|---|---|---|
| Employer | 88 | 18% |
| Employer Representative | 46 | 9% |
| Charity | 47 | 10% |
| Trade Union | 17 | 4% |
| Occupational Health Provider | 35 | 7% |
| Health Service Provider | 23 | 5% |
| Self-Employed | 16 | 3% |
| Individual | 111 | 23% |
| Other | 102 | 21% |
| Total | 485 | 100% |
As Figure 1 demonstrates, of those employers who responded, the majority were large employers (43%), followed by small (23%) and medium sized employers (23%) and finally micro-employers (12%). Broken down by industry, the majority of respondents said they provided ‘other services’ (37%), followed by ‘public admin, education and health’ (29%) and construction (9%). Respondents classifying themselves as ‘other services’ included a wide range of organisations and individuals, including membership associations, insurance providers, professional bodies, patients, employees and unemployed people.
Figure 1: Charts illustrating employer responses by size and type
| Size | Percentage |
|---|---|
| Micro (0-9 employees) | 12% |
| Small (10-49 employees) | 23% |
| Medium (50-249 employees) | 23% |
| Large (250+ employees) | 43% |
| Sector | Percentage |
|---|---|
| Private | 63% |
| Public | 23% |
| Voluntary | 14% |
| Region | Percentage |
|---|---|
| North East | 7% |
| North West | 11% |
| Yorkshire and the Humber | 7% |
| East Midlands | 8% |
| West Midlands | 9% |
| East of England | 8% |
| London | 11% |
| South East | 13% |
| South West | 8% |
| Wales | 7% |
| Scotland | 7% |
| Northern Ireland | 3% |
| Industry | Percentage |
|---|---|
| Agriculture, forestry and fishing | 1% |
| Energy and water | 1% |
| Manufacturing | 7% |
| Construction | 9% |
| Distribution, hotels and restaurants | 4% |
| Transport and communication | 7% |
| Banking and finance | 4% |
| Public admin, education and health | 29% |
| Other services | 37% |
In addition to the responses received via the online portal, some responses were submitted separately by stakeholder organisations. These responses provided comment on the package of measures as a whole or individual policy areas relevant to the stakeholder organisation, rather than responses that followed the ordering of questions included in the consultation document.
Government also hosted 12 roundtable events across the UK to promote engagement with the consultation, as well as 6 insight groups focusing on specific policy areas. These insight groups considered the right to request workplace modifications, SSP and OH.
Finally, government received 772 responses from Mind, the mental health charity, which distributed specific consultation questions to its membership base and invited members to respond.
Across these different sources, the responses received were comprehensive and rich in detail. The consideration respondents exhibited has enabled government to understand both the broad trends and nuanced comments underpinning consultation feedback.
In the context of the COVID-19 pandemic government took additional time to consider responses to ensure the package of measures being proposed remained relevant in a post-COVID-19 landscape. Government is confident that this package of measures is more relevant than ever.
Chapter 1 outlines our plans to support employers to navigate the work and health landscape. Chapter 2 outlines our plans to support employers and employees during sickness absence. Chapter 3 outlines responses to the consultation on SSP reforms. Chapter 4 outlines our plans to help employers deal with cases where they need additional high-quality OH support. Finally, Chapter 5 concerns other issues raised during the consultation, including enabling better use of the fit note, the role of insurance, tax and Access to Work (AtW).
Chapter 1: Helping employers navigate the work and health landscape and make better use of existing tools
This government wants employers and employees to have better interactions about work and health to support employee retention. We want to mitigate any adverse effects of the pandemic (whether direct or indirect) on disabled people or people with long-term health conditions.
Both employers and employees told us that navigating the variety of sources of publicly-funded advice and information on work and health is confusing. Government heard that providing easily-accessible information and advice is important, as some employers report lacking confidence and being afraid of ‘doing the wrong thing’. This is particularly true for SMEs, many of whom do not have access to dedicated HR support and/or in-house OH (see Chapter 4). [footnote 28]
Government also heard that there is a lack of awareness and understanding of rights and responsibilities under the Equality Act among both employers and employees, in particular around providing reasonable adjustments.[footnote 29]
It is vital that employers (including the self-employed) have access to the right tools and information to enable them to effectively support their employees and reduce the risk of people falling out of work in the long term.
Recognising what employers need
Employers have an important role to play in creating healthy and inclusive workplaces, but often lack the time, resources or expertise to take the right steps (especially among SMEs).[footnote 30][footnote 31] This exposes employers to legal and reputational risks, productivity losses and increased costs. Some recruitment practices mean that disabled candidates or applicants with long-term health conditions don’t always get fair consideration. Existing employees do not always get the support they need to stay in work. This contributes to the lower rates of employment for disabled people and the wider problem of health-related job loss, some of which could be prevented.
COVID-19 has shone a light on a range of health-related issues that preceded the pandemic. Navigating the challenges raised by COVID-19, and the changes this brings to the management of health in every workplace, has increased employers’ information needs. These include how to support flexible/home working, how to support people with long-term health conditions (including mental health conditions) in the workforce, how to manage returns to work and how to ensure that workplaces are safe. Government has already issued clear guidance documents to help employers adapt, including the suite of ‘Working safely during Coronavirus’ guides aimed at different types of work.
While employers see central government as the most reliable information source, they report that the current information offer is fragmented, hard to navigate and difficult to apply in practice. They want support that helps them to solve real-world problems. Research shows that providing better information and advice can improve take-up of health and wellbeing initiatives amongst SMEs.[footnote 32]
A stronger information offer for employers will underpin and support the other elements of the consultation package, as well as existing government support and advice (including Disability Confident, SSP and other related content ‘owned’ by ALBs and other Departments). Without this, take-up of other consultation measures is likely to be limited and it will be difficult to realise their potential benefits in full.
Improving the offer
The government proposed to improve the provision of advice and information to support management of health in the workplace and encourage better-informed purchasing of expert-led OH advice (see Chapter 4 for more details on the latter).
Government heard that although employers access the internet, they experience navigation issues when searching for information on health in the workplace, and also aren’t sure what information they can trust. They want information that is good quality, easily accessible and in one place.
Government’s online information is the preferred starting point for many employers, in particular SMEs. Employers said they trusted government advice and guidance more than other information sources. They were supportive of a one-stop government information service where resources were better integrated.
Many employers stated they require more information, advice or guidance on dealing with disability and long-term health conditions. There was a strong consensus for better quality and more accessible information.
Consultation responses also underlined the importance of providing locally focused information and using local networks to support employers. A number of projects and trials have been running across DWP and other Departments, as well as external to government, to research and identify how we can most effectively meet these needs.
What government intends to do next
Government will ensure that better integrated health and disability-related information for employers is made accessible. We will:
- continue collaboration between teams producing content in different parts of government and across ALBs to enhance resources to support COVID-19 returns to work/workplaces
- develop a national information and advice service for employers on health, work and disability, with material designed to help manage common health and disability events in the workplace. This will be developed with the needs of SMEs in mind
On the proposal for a national information and advice service, government has been working with employers to understand their needs. This is informing design work during 2021.
Chapter 2: Helping employers improve support for employees during sickness absence and return to work
Government plans to help employers navigate the work and health landscape, make better use of existing tools and equip them with the right information and advice to support employees’ needs which should inform better interactions around work and health. In many cases these good conversations between employers and employees will facilitate an employee remaining in (and returning to) work.
However, it is not always the case that employees receive the support they need from employers. That is why government considered proposals aimed at helping all employers understand what they should do to support employees when sickness absence happens. This chapter covers the importance of workplace adjustments and proposals to strengthen statutory guidance to encourage early and supportive action from employers.
Concerns have been raised that COVID-19 has exacerbated some of the existing issues around work(place) adjustments that were highlighted by consultation respondents, specifically around awareness, understanding and compliance. There are reports that the large number of people working differently has led to some employees not receiving adjustments in new work settings, for example when working from home, and that some employers lack the knowledge needed to provide them in this new context. With emerging evidence from early on in lockdown suggesting a marked increase in the number of employees with worse symptoms of musculoskeletal pain, higher levels of fatigue, poor sleep, and higher levels of eye strain, the number of people who are entitled to – or would benefit from – work(place) adjustments could be increasing.[footnote 33]
The importance of adjustments
As the consultation set out, effective work(place) modifications and adjustments (for example, changes to the working environment, hours and tasks, as well as phased returns to work) can reduce the length of sickness absence and help employees remain in work. The consultation sought views on whether to introduce a right to request work(place) modifications on health grounds in order to increase the number of people able to benefit from such modifications and adjustments. It also sought views on how this might be implemented. The consultation also made clear that the introduction of this new right was not intended to have any adverse impact on the existing duty to make reasonable adjustments for disabled people under the Equality Act 2010.
Overall, consultation responses agreed that a new right could be an effective way to help employees; however, respondents also raised significant concerns which broadly broke down into the following main themes:
Lack of awareness and understanding
Government heard that there is a lack of awareness and understanding among employers and employees around their existing rights and responsibilities. Specifically, there were particular issues around the definition of ‘disability’ and concerns that individuals may not be aware of what they are entitled to under the act. Disagreement between employers and employees over whether or not an individual is covered by the act was raised.
Government also heard that employers may struggle to identify appropriate adjustments and what constitutes ‘reasonable’ under the duty to make reasonable adjustments. This was highlighted as an area of particular concern for SMEs.
A number of responses therefore urged government to do more to increase awareness and understanding of existing rights and responsibilities in this area, either in addition to or instead of introducing additional legislation. For example, one respondent suggested implementing awareness campaigns to educate employers and employees.
Mental health was raised by a number of respondents as an area requiring greater awareness and understanding. Some respondents proposed changing the definition of disability in the Equality Act to better support those with mental health and fluctuating conditions.
Risk of greater confusion
A number of responses expressed concern that introducing a new right to request work(place) modifications on health grounds risked causing greater confusion among employers and employees in what is deemed an already complex area. There was general concern that introducing new legislation in this area would risk ‘muddying the waters’.
Risk of undermining existing workplace protections
A lot of responses raised concerns that introducing a new right to request work(place) modifications on health grounds could risk undermining existing workplace protections, in particular the duty to make reasonable adjustments for disabled people. Respondents were concerned that in practice, introducing the new right may lead to employers shifting focus from their positive duty (to make reasonable adjustments) to the worker’s right to request work(place) modifications.
Others highlighted the risk of employees who are unaware of their statutory rights under the act being less likely to receive reasonable adjustments as a result of lack of knowledge or being influenced by employers. There was particular concern amongst some respondents that a new right could legitimise refusing a request under the act and might limit the ability of disabled employees to seek the reasonable adjustments to which they are legally entitled.
Compliance
Government heard there are issues with the way in which some employers approach the legislation, with some respondents citing examples of employers creating organisational barriers for disabled employees to access their rights. They also indicated employers are more likely to make reasonable adjustments for those employees that are more ‘valued’ to the business. A number of respondents stated that the intent of our proposal would be better achieved through strengthening existing protections under the act.
What government intends to do next
Given the risks identified of introducing new legislation in this space and feedback on the issues with the existing framework, on balance, government has decided not to proceed with the introduction of the proposed right to request work(place) modifications at this stage. However, there is a strong case to consider what more could be done to raise awareness and understanding among employers and employees of their existing rights and responsibilities, in relation to both the duty to make reasonable adjustments and work(place) adjustments more broadly.
The Equality and Human Rights Commission (EHRC) is the enforcer of the Equality Act, which includes the reasonable adjustments duty. It undertakes strategic litigation and enforcement to challenge flagrant, systemic and egregious breaches, or to clarify the law. The Commission is resourced to undertake strategic enforcement of EA10 (so individuals will usually need to make an Employment Tribunal claim to challenge a failure to make reasonable adjustments).
The EHRC produces guidance and resources for employers, service providers and other duty bearers to encourage compliance. It has introduced additional guidance for employers on how reasonable adjustments should be made during the COVID-19 pandemic, including several examples of specific adjustments to encourage good practice. The government will continue to support and fund the Equality Advisory and Support Service (EASS), the helpline which provides free bespoke advice and in-depth support to individuals with discrimination concerns. The EASS has the ability to intervene on an individual’s behalf to help resolve an issue, including in relation to reasonable adjustments at work, and can provide advice on whether a person is likely to meet the Equality Act’s definition of disability. The EASS can also advise people who wish to take their complaint further on their options.
Access to Work (AtW) may also provide funding to meet additional employment costs resulting from an individual’s disability (or long-term health condition) that are over and above those that may be considered reasonable under an employer’s duty to make reasonable adjustments.
Moving forward, Chapter 1 outlines our plans for better-integrated health and disability-related information and advice for employers, which will include material designed to help employers manage common health and disability events in the workplace. This will in particular be useful for SMEs, who often do not have dedicated HR functions.
Chapter 5 discusses Access to Work (AtW). AtW recognises the need to raise the visibility of the support it offers and is working to expand its reach by proactively raising awareness of AtW with disabled people, those with long-term health conditions and employers. This has included a communication campaign and social media activity.
DWP is working to transform AtW to deliver a modern, streamlined service that provides an improved customer experience. This includes introducing a new digital customer journey that will deliver a quicker and more efficient service. To enable disabled people to have greater flexibility to work from more than one location, AtW has introduced a new flexible offer to respond to the challenges of Covid-19, and to support disabled people to take up opportunities. Building on this flexibility and to support transitions into employment, AtW is piloting a new Adjustments Passport for young people who are transitioning from education to work, veterans leaving the armed forces, and freelancers and contractors moving between job roles.
Alongside our contribution to the COVID-19 Mental Health and Wellbeing Recovery Action Plan, we will continue to support the business-led work with the Thriving at Work Leadership Council, to promote best practice and guidance offered via the Mental Health at Work online gateway. This hosts over 400 resources to inform and advise employers on managing mental health in the workplace.
In addition, flexible working has the potential to help improve retention of staff who may otherwise fall out of work due to a (temporary or permanent) change in their health. The Department for Business, Energy and Industrial Strategy (BEIS) is taking forward the 2019 Conservative Party manifesto commitment to encourage flexible working and to consult on making it the default unless employers have good reasons not to. The consultation will be published in due course.
These steps, as well as wider measures outlined in this response, including our plans to improve access to OH outlined in Chapter 4, will help encourage more adjustments to be made for disabled people and those with long-term health conditions and help improve compliance with the reasonable adjustments duty. This will help people to either stay in work or return to work following sickness absence. Government will continue to work across departments and with external stakeholders, including the EHRC, to consider other ways to raise awareness and understanding among employers and employees.
Strengthening guidance to encourage early and supportive action from employers
In 2018 around 1.4 million people experienced LTSA, defined as a leave of absence for four or more weeks, resulting in over 100,000 people falling out of work. Of these, 25,000 fell out within the first six weeks.[footnote 34] We know that early intervention and support during sickness absence is important and that a lack of support from an employer can be a key factor in prolonging sickness absence.[footnote 35][footnote 36]
Although research suggests that the majority of employers reported putting measures in place to manage their employees’ return to work following a LTSA, this is not universal (e.g. 79% had used regular meetings and 69% had developed return to work plans).[footnote 37] There were also differences between large and small employers, with large employers being more likely to report adopting a wider variety of measures. Evidence also suggests that some individuals may be dismissed instead of effort being made to support them back into the workplace.[footnote 38]
COVID-19 has further highlighted the importance of maintaining best practice, with lockdown measures having a potentially significant impact on health and wellbeing.[footnote 39] Early research suggests that the sudden changes to homeworking due to the pandemic has contributed to an increase in musculoskeletal conditions and poor mental health for some employees, especially among those in less frequent contact with their employer and also younger workers.[footnote 40]
The consultation asked whether statutory guidance should be strengthened to encourage employers to take appropriate steps to support a person on sickness absence to return to work, and sought to establish whether this guidance should be principle-based or set out specific actions for employers to take.
The majority of respondents agreed that statutory guidance should be strengthened, stating that clear guidelines would give employers more confidence to act and provide consistency in their approach. Of those who did not agree, government heard concerns over increased business burdens and reduced flexibility, should the statutory guidance be too prescriptive. Respondents who said ‘maybe’ agreed to strengthened statutory guidance providing the guidance acknowledged individual circumstances and recognised that employees should be given an appropriate amount of time to recover before actively engaging in a return to work.
A prescriptive vs. principle-based approach
The majority called for a combined approach: broad statutory principles supported by non-statutory detailed information and case studies for those who may need additional support.
Responses suggested the majority of large employers have processes in place for sickness absence management. However smaller employers are less likely to have these processes and therefore struggle when sickness absence occurs. To overcome this, smaller businesses were more likely to prefer prescriptive guidance on what actions to take to support an employee returning to work following sickness absence, to help avoid mistakes and potential grievances against them. However, concerns were raised that a heavily prescriptive approach could inadvertently create a ‘tick list’ to dismissal.
Government also heard that strengthened guidance combined with clear principles will offer transparency on what should be expected during sickness absence, both from the employer and the employee. However, this should not be unduly prescriptive and should not cut across the collaboration needed between employers and employees to respond to the individual set of circumstances.
Consistency in engagement
A common theme emerged from employees around a lack of consistency with the support they received and the documentation of key meetings and actions. Similarly, employers noted the same issues with consistency and called for better quality and more accessible advice to help them provide a consistent approach and meet legal requirements.
Responses also highlighted the importance of employee engagement. Equal weight was given to identifying barriers, agreeing return to work plans and engaging with OH services, suggesting that the more collaborative the approach between the employee and employer, the greater the likelihood of agreeing appropriate next steps to aid a more sustainable return to work.
What government intends to do next
Government recognises that employers need more clarity on their existing responsibilities and clearer information to enable them to support disabled people and those with long-term health conditions to remain in work or return to work following sickness absence.
Therefore, Government has asked the HSE to explore ways to strengthen guidance on how employers can best support disabled people and those with long-term health conditions to remain in work, and on managing related sickness absence. HSE already provide a range of expert advice to support employers in the area of health and work, including preventing and managing work-related stress and musculoskeletal disorders: two of the leading causes of sickness absence.[footnote 41]
Supporting disabled people and those with long-term health conditions to remain in work and managing any related sickness absence requires a collaborative approach across government. As a first step, working with other ALBs, HSE will strengthen existing non-statutory guidance before exploring the introduction of statutory guidance.
Government recognises that employers report barriers to supporting employees to return to work following sickness absence. Small employers in particular report a lack of time or staff resources and capital to invest in support. Existing government schemes such as Disability Confident and Access to Work can help employers to support disabled employees and those with long-term health conditions. In addition, employers can draw on the expertise of the existing OH market which can help individuals’ return to work and reduce unnecessary sickness absence. The measures outlined in this consultation response build on this support.
In particular, our plans for a national information and advice service for employers on health, work and disability; OH market reform, including increasing access for SMEs; and changes to the fit note to encourage better work and health conversations will help employers adhere to the key principles of the guidance.
Chapter 3: Statutory Sick Pay
The consultation sought views on reforming SSP so that it is available to all employees that need it, more flexible in supporting returns to work, and underpinned by a suitable enforcement framework. In response to COVID-19, government has introduced a series of unprecedented measures to ensure that individuals and businesses have access to the support they needed. Access to SSP has been a key part of this response. Government extended eligibility of SSP to employees who were self-isolating in line with public health advice, ensuring that eligible employees were not without this financial protection. We also introduced the Coronavirus Statutory Sick Pay Rebate Scheme, which supports small and medium sized businesses throughout the country to manage the increased costs of covid-related absences, and we temporarily suspended waiting days which made SSP payable from the first day of a coronavirus-related sickness absence.[footnote 42]
Phased returns to work: enabling flexibility
The consultation outlined the benefits of phased returns to work which have been shown to reduce the likelihood of an individual falling out of work and increase the time spent at work in the long-term. They have been shown to be particularly effective in supporting individuals with musculoskeletal and mental health conditions, which are the most common health conditions of disabled people both in and out of work.[footnote 43][footnote 44]
Under the current rules, SSP does not allow for phased returns. Payment of SSP stops when an employee returns to work, even if they return on reduced hours. This can deter employers from offering phased returns and employees accepting them. Respondents were broadly supportive of phased returns to work. There was unequivocal support for clear information and guidance on phased returns, including in relation to implementation across settings and examples of scenarios in which a phased return could be beneficial.
Respondents were supportive of more guidance from healthcare professionals, for example via the fit note. The “maybe fit” section on the fit note, which includes the option of a phased return, is currently underutilised by GPs, with only 7% of fit notes referencing this option.
The Lower Earnings Limit
Employees who earn less than the Lower Earnings Limit (LEL), which is currently £120 per week, do not qualify for SSP. This includes those who have multiple jobs which are each paid below the LEL. Government did not extend SSP to employees below the LEL as part of its response to the pandemic. Extending SSP in this way would not have been the most efficient way to support these employees and would have placed an immediate cost on employers at a time where most required government support. The most effective way of getting financial support to these individuals was through the Coronavirus Job Retention Scheme and the existing benefits system. As part of the response to the pandemic, government took steps to strengthen the safety net including through increases to Universal Credit.
The consultation asked whether respondents agreed that SSP should be extended to employees earning below the LEL and views on the rate that should be extended to this group. A majority of respondents (75%) agreed that SSP should be extended to employees earning below the LEL. This measure was supported by small and large employer respondents alike. Respondents felt that by extending SSP to those earning below the LEL, employers would be better incentivised to reduce sickness absence for all of their employees.
Supporting SMEs with the cost of sickness
It is important that sick pay is paid by the employer in order to ensure there remains a strong link to the workplace and to incentivise the employer to support a return to work. The consultation acknowledged that SMEs may be less likely to have the financial and human resources to invest in health and wellbeing initiatives such as occupational health provision. Despite this, many SMEs already adopt good practice measures such as phased returns to work following absence.[footnote 45]
In response to COVID-19, government introduced a temporary rebate to support SMEs with the increasing cost of absence as significantly more employees were required to take sickness leave in line with public health guidance. This rebate was focussed on supporting SMEs with the costs of increased absence caused by periods of self-isolation, rather than driving better management of absence. Take up of the scheme has been lower than initially forecast.
The consultation sought views on how a permanent rebate could support employers to manage the cost of sickness absence and encourage best practice. Responses to this were mixed. Most who favoured a rebate supported ease of access over any attachment of conditions, whereas others suggested that a rebate should be linked to outcomes such as a return to work. A key concern from respondents was that this sort of conditionality could lead to perverse incentives for employers to bring employees back to work before they were ready. Respondents felt that linking a rebate to a code of practice or other guidelines would result in a ‘tick box’ exercise and lead employers to adopt the minimum standards required to qualify for a rebate rather than innovating to reduce sickness absence.
Enforcement
An effective enforcement system is vital to creating a level playing field for business and employees alike. There are indications that some employees are not receiving SSP when they are entitled to it, but instead relying on welfare benefits. Respondents felt that government should be taking a more robust approach to enforcement and cracking down on employers who fail to meet their obligations. The majority (72%) agreed that there was a need to introduce better enforcement of SSP.
Government remains committed to the development of a Single Enforcement Body which will bring together existing enforcement bodies into a single and recognisable organisation. The Body will protect workers across the country and help to provide a level playing field for the majority of employers who respect the law. As part of the consultation response on the Single Enforcement Body, government confirmed its intention to include enforcement of SSP within the Body.
A consistent theme throughout the consultation response was a need to not penalise employers who had made genuine mistakes. In practice, it can be difficult to establish whether a genuine mistake has been made and so enforcement should take a proportionate approach with a focus on rectifying the problem and supporting future compliance.
Next steps
The consultation posed several important questions on the future of SSP which require further consideration.
Government maintains that SSP provides an important link between the employee and employer but that now is not the right time to introduce changes to the sick pay system.
Chapter 4: Helping employers access quality Occupational Health (OH) support
Expert support such as OH services can be a critical component in helping individuals remain in and return to work, reducing unnecessary sickness absence, increasing productivity and enabling individuals to live better for longer. In this document where we refer to OH services we include services that can help to achieve these (and other relevant) outcomes and reduce ill-health related job loss. These can include fitness for work assessments, health surveillance, advice on return to work and reasonable adjustments, vocational rehabilitation, case management, biopsychosocial approaches[footnote 46], health and wellbeing services and signposting to services that treat specific conditions. While in many cases action such as better work-focused conversations between the employer and employee is enough to support job retention (see Chapter 1), in others, additional high-quality support is required to prevent people falling out of work.
Government believes OH has an important role to play in supporting job retention, and enabling staff to thrive in work. This has been underlined by the role that OH services have played in the COVID-19 recovery, supporting returns to work. Research conducted by the Society of Occupational Medicine (SOM) during the early stages of the crisis showed over three quarters of NHS OH providers and more than half of in-house OH providers said their workloads had increased.[footnote 47]
However, there is a wide variation in access to OH services. Large employers are five times more likely to offer OH than small employers.[footnote 48] While employees for small employers are less likely to have long-term sickness absences than employees of large employers, disabled people working for small employers are more likely to lose their job, as the gap in job retention rates between disabled and non-disabled people is bigger in small employers than large employers.[footnote 49] Over a third of employers who do not access OH services cite cost as the main barrier, but knowledge of actual costs amongst small employers is limited[footnote 50] and some employers without access have a lack of understanding, or have not fully considered the benefits, of OH services.[footnote 51] Some see OH services as relevant only to those who have to deal with long-term sickness absences or disabled employees or those with health conditions, and sometimes as a means for managing people out of organisations.[footnote 52] Government research indicates that both providing financial incentives and/or providing advice in the form of a needs assessment and signposting could increase SME take-up of health and wellbeing services such as OH.[footnote 53]
One of the aims of the new information and advice service in Chapter 1 is to ensure all employers are better aware of the broader benefits of OH for all employees and their productivity, as opposed to just those experiencing sickness absence or with a long-term health condition or disability. However, increasing employer awareness and understanding of OH alone is not enough.
‘Health is everyone’s business’ identified several issues in the commercial OH market, which currently delivers the majority of OH services. These included: cost as a key barrier to procuring OH; shortages in the OH workforce, particularly clinical staff, which risk the future capacity of the OH providers to deliver services; potential for more rapid innovation particularly targeted at SMEs and self-employed people; and a lack of awareness/understanding of the full range of OH services.
The measures outlined in this chapter form a strategy for reforming the OH landscape of provision, both to increase demand for OH and address these issues. This strategy, combined with the measures outlined earlier in this response – including improvements to information and advice (Chapter 1) and encouraging and supporting employers to take early action to support employees (Chapter 2) – will support development of a market that has the capacity and capability to respond to increased demand, particularly in light of COVID-19.
The impact of COVID-19 on the OH market
Alongside analysing responses, government has carefully considered how COVID-19 has affected the OH market.
An independent market forecast predicts the ‘new normal’ will present opportunities for the OH sector from 2021 onwards. These could result from the need for employers to be more proactive in managing health in the workplace and employees exhibiting greater concern over their health and safety at work. Technological OH developments are forecast to be crucial for penetrating the SME market and ensuring OH services can reach employees working remotely.[footnote 54]
A survey by the Society of Occupational Medicine (SOM) conducted in April 2020 showed three quarters of practitioners were spending an increased amount of time providing remote consultations – via both telephone and video software such as Zoom/Skype – with almost all respondents reporting a decrease in face-to-face work, reflecting behavioural changes evident across workplaces during the pandemic.[footnote 55]
Recent research commissioned by DWP also showed up to an additional 8% of businesses newly purchased OH during the pandemic specifically to help them deal with COVID-19-related OH issues.[footnote 56]
Evidence has shown the challenges businesses continue to face in achieving pre-COVID-19 growth and revenue levels. A survey conducted by the Bank of England shows that in Q4 2020, businesses’ sales, employment and investment levels were lower than expected in the absence of COVID-19, and that businesses do not anticipate investment to recover until at least 2022. The survey also found that implementing measures to control the spread of COVID-19 were expected to increase costs of running the business.[footnote 57]
The pandemic has made the proposed strategy for reforming the commercial OH market more important than ever. The strategy outlined in this chapter will help improve employer access to relevant OH services, by: testing a potential new OH subsidy to help tackle financial barriers to purchasing OH; supporting the development of innovative OH services which may improve access for those currently less likely to purchase OH (meaning SMEs and self-employed people); developing the infrastructure to support continuous research and development in OH; driving continuous quality improvement in the market; providing access to procuring support that can help employers purchase relevant quality services that meet their needs; and addressing capacity issues in the OH workforce to ensure a range of specialities are available in the long term to serve the anticipated increase in health conditions post-COVID-19.
A potential new OH subsidy
The consultation sought views on whether a targeted financial incentive would help SMEs and self-employed people to overcome barriers to accessing OH. Views were also sought on how this might be administered and what services should be prioritised under a subsidy. A subsidy would aim to:
- increase access to OH services by reducing purchasing cost for SMEs and self-employed people, targeting those least likely to have access
- encourage more employers to take a proactive approach in supporting health in work and to purchase OH through the commercial market
- support the growth of a dynamic independent sector to stimulate more affordable offers for SMEs and the self-employed
Overall, a majority of respondents were in favour of a subsidy for SMEs and the self-employed to increase access to OH. Employers being asked to contribute part of the cost was thought necessary to ensure their commitment and to protect against exploitation of the scheme. Only a few respondents were directly opposed to the proposal and expressed opinions that OH should be free, or should form part of NHS care. Some respondents highlighted the importance of a subsidy being easy to access and drew attention to the impact on business of administrative processes as well as the availability of OH services.
The consultation sought views on giving the smallest SMEs and self-employed people the largest subsidy. Most respondents favoured this approach, with others undecided and a small number opposed. Respondents expressed views that eligibility should be means tested or based on turnover, a uniform entitlement would be simpler, and tax incentives would be more inclusive of all employers.
The consultation asked what type of OH services should be prioritised by any subsidy. Advice and assessments were most often the first priority, well ahead of training and capability of managers and businesses provided by OH professionals, and OH recommended treatments. However, treatments were often the second highest priority, showing they are still highly valued.
Consultation views and feedback from the Occupational Health Expert Group (OHEG) suggested government should look beyond traditional OH medicine to include other tools that would also help employers retain employees with disabilities and long-term health conditions, such as vocational rehabilitation and case management.
The consultation sought views on measures to ensure subsidised services were of sufficient quality. The most common proposals were to ensure that providers are registered or accredited, such as signed up to a regulatory body, and to have an approval identifier such as a licence or membership of an independent accreditation scheme such as Safe, Effective, Quality Occupational Health Service (SEQOHS). Respondents also mentioned that there should be a feedback mechanism and emphasised the importance of having access to a wide range of providers.
Government believes linking quality requirements to a provider’s eligibility to deliver subsidised services could incentivise providers to continue to offer a good standard of service, and support quality improvement in the market. Responses from OH providers expressed mixed views about how demanding these requirements should be.
Some providers suggested that a subsidy should be underpinned by registration or accreditation schemes, whilst others favoured ‘lighter touch’ options such as an audit process, a benchmark or standards indicator, a national register of minimum requirements, or a government approved list of providers.
There is evidence of self-regulation amongst providers, with almost all OH providers agreeing that the training, development and/or accreditation systems they had in place were effective in ensuring quality of service.[footnote 58] Further detail on proposals specifically related to quality and buying support are included below.
What government intends to do next
Government will test a subsidy which would aim to gather evidence on whether targeted financial incentives improve access to OH and employment outcomes. This test will be robustly evaluated and findings, alongside developments in OH reform policies, and affordability, will inform the case for potential fixed term roll-out in the future. Government will work with experts to ensure minimum qualification criteria are in place that OH providers should meet in order to be able to deliver subsidised services, and will assess provider suitability criteria as part of the subsidy test.
These criteria should balance the need for employers to have confidence in the services they are procuring, with the importance of ensuring sufficient choice is available in the market and that innovative practice is encouraged.
The aim would be to coordinate testing to align with developments in employer information and advice as well as wider OH market initiatives to develop buying support and innovation.
Government has met with OH experts and reviewed evidence from the Fit for Work programme to consider how best to design and deliver a subsidy test that is effective and does not impose unnecessary administrative burden on employers.
Government is continuing discussions with representatives of the insurance sector, which will help in understanding the different routes through which employers may prefer to access OH services.
Quality and buying support
The consultation package aims to encourage many more of the smallest employers and the self-employed to use OH. Many such employers will have no awareness or experience of procuring or using OH. There is limited guidance targeted at SMEs and self-employed people that either makes the case for OH or provides advice about when and how to procure it effectively. This increases the risk that they will purchase inappropriate or poor value services, or decide against procuring OH at all.
There is also a need to improve the knowledge of purchasers in ways that will encourage the market to compete (on both price and effectiveness of service), while ensuring continual development and provision of good quality, cost-effective services, especially for the SME sector.[footnote 59]
The consultation set out proposals to improve the advice and information support, both at national and local level, for employers (especially SMEs and self-employed people) on workplace health and wellbeing. This included improving access to information, such as on how and where to access OH services, which could improve employers’ confidence in purchasing expert-led work and health services.[footnote 60][footnote 61] This guidance should be relevant and user-friendly, especially for SMEs, in order to improve employers’ confidence in dealing with health-related work issues.
The consultation also discussed proposals to encourage standards and indicators of quality, including ones which focus on the quality and cost effectiveness of the services that employers receive.
Improving buying support
The consultation asked what additional information employers would find useful when purchasing, or considering purchasing, OH. Respondents were generally supportive of the need to improve the buying support available. Employers (of all sizes) supported a range of measures. From most popular option to least popular, these measures were:
- a toolkit that could include information on OH referral and assessment processes
- a provider database
- an online questionnaire to help employers identify what type of services they could benefit from
- a comparison website
- information on the value of OH services
- basic online information on the process of procuring OH services
Government heard smaller employers would find basic online information about the process of procuring OH services more helpful than large employers, while micro employers and OH providers prioritised an online questionnaire that would help employers identify the types of services they could benefit from.
Improving quality
The consultation asked what indicators of quality and compliance arrangements would help employers to choose providers and improve the standard of services.
A range of quality indicators were supported by respondents. There was particular support from employers and OH providers for developing indicators with a closer or direct link to outcomes. Suggestions for outcome indicators included sickness absence, staff retention, satisfaction levels, return to work rates, and work modification implementation among others.
Several responses noted the need to ensure outcomes are measured in a robust and consistent way, and suggested that caution should be taken when using absence data as a metric on its own because changes in sickness absence rates may be influenced by a number of factors. A clear theme also emerged that outcome-linked indicators should start with better collation of data.
The majority of SEQOHS (Safe Effective Quality Occupational Health Service) members considered a SEQOHS accreditation as the best overall indicator of quality in the OH market and some respondents highlighted a potential opportunity to link into a review of SEQOHS.[footnote 62]
What government intends to do next
Building on the feedback from respondents, and linked to the national advice and information service (outlined in Chapter 1), Government is undertaking further design work with SME employers and self-employed people on how best to improve the process of choosing quality and cost-effective OH that meets their needs.
Government is interested in the potential for outcome-linked metrics to support continual provider improvement and employer choice. Given the considerations highlighted above, developing outcome-linked metrics is a longer-term challenge, but there may be short-term opportunities to make progress, and government is working with stakeholders and providers to explore these issues further.
Government has undertaken feasibility work with the NHS Getting It Right First Time programme (GIRFT) which is delivered in partnership with the Royal National Orthopaedic Hospital and NHS England and NHS Improvement. GIRFT has experience using data and outcomes metrics to support sharing of best practice in the NHS. As a first step, government is working with GIRFT to pilot a best-practice methodology for collection of outcome metrics and to consider solutions to implement, build on and scale this methodology, as well as explore how employers might use data and outcomes to understand the value of occupational health.
Government is working with the Faculty of Occupational Medicine (FOM) as part of the FOM’s ongoing review of the SEQOHS standards and accreditation of services. Government has expressed its interest in the review exploring opportunities for SEQOHS to introduce stronger links with outcomes, and to increase engagement with employers and smaller providers.
Innovation in Occupational Health (OH)
The previous sections outline government’s strategy for increasing employer demand for and access to OH. Alongside this, another crucial part of the strategy is to ensure the sector has the capability and capacity to respond to new increases in demand. One approach to creating more capacity in the market is to address OH workforce shortages (see next section). As key elements of this approach – such as training new OH doctors and nurses – will take time, it is important to ensure other complementary methods of boosting capacity are available so the sector can rapidly respond to increases in demand. Innovation – defined as investing in new or improved services, delivery methods or technologies – can be an effective solution which can also help drive increased employer demand, particularly from groups who are less likely to purchase OH (such as SMEs and self-employed people). Government is exploring proposals that aim to increase the pace of innovation and establish the long-term structures to drive the development of services that support job retention.
Increasing the pace of innovation and supporting the market in the long term
The consultation invited views on government providing dedicated funding for innovations that could increase access to OH for SMEs and the self-employed, two groups currently less likely to purchase OH.
The consultation also sought views on how best to tackle some of the limitations identified in working age health research, including the need to improve research prioritisation, to better co-ordinate research funding – with a particular focus on promoting multi-disciplinarity – and to improve dissemination and knowledge translation, ensuring research findings are used to improve service provision.
The proposals aimed to ensure the market has the tools to innovate more rapidly and maintain this over the long term. Recent government research conducted with OH providers highlighted that while cost efficiencies and a desire to provide high-quality services to customers drive OH providers to innovate, many smaller OH providers lack the capacity or formal structures to innovate.[footnote 63] The innovation proposals aim to help OH providers overcome these challenges and drive rapid, long-term innovation.
Some of the measures outlined earlier in this response will also help OH providers overcome some of the broader challenges they say they face when seeking to innovate. For example, the information and advice (Chapter 1) and buying support (Chapter 4) proposals may increase employer demand for OH by raising employers’ awareness of the benefits of OH services. Similarly, the workforce proposals outlined in the following section may create additional capacity in the market, helping OH providers who recruit additional staff spend more time on innovation.[footnote 64]
Dedicated funding to drive innovation
Responses indicated that there is a case for providing funding or other support to OH providers to encourage engagement in research and innovation. A majority of respondents agreed access to finance and help with innovation/evaluation would help OH providers increase the pace at which they innovate.
Funding was not the only barrier identified to innovation. Some responses said protecting Intellectual Property Rights (IPR) can be a concern for OH providers, as can the time it takes to apply for funding from existing innovation opportunities, given that this takes time away from fee-paying work. Some responses also said other support is required to help providers innovate (for example, access to innovation expertise).
Similar themes were evident in recent government research exploring innovation in OH. Capacity and cost were identified as the main barriers to innovating, with providers also highlighting that the way the market operates (with a tendency to commission based on price rather than quality) contributes to many providers approaching innovation in a reactive rather than a proactive way, responding to customers’ demands rather than seeking new ways to offer services or improve efficiency.[footnote 65]
Other barriers to innovating identified in the consultation responses included:
- legal consent and General Data Protection Regulation (GDPR) limiting OH providers’ ability to share information easily between organisations, thus acting as an inhibitor to those seeking to offer multidisciplinary services
- challenge of generating returns from SMEs and the self-employed due to the difficulties in trying to achieve economies of scale
Responses suggested that government should focus on new OH service models and technology to increase access to OH for these groups.
Examples of the former could include group purchasing approaches, where a centrally funded OH provider is geographically responsible for a number of business parks, with employers located on the parks paying different rates into an overall ‘pot’, enabling them to access different models of OH (for example, standard or premium services). This could create economies of scale and reduce the cost of purchasing per employer, as they are effectively risk-pooling resources.
New technology could be used to provide digital support services, to support effective triage of individuals or to run services in new ways and spend less time on administrative tasks. This would then increase the provider’s capacity to take on more clients.
Improving the research infrastructure that supports innovation
Responses showed widespread support for improving the research infrastructure that supports innovation, including tackling the research problems identified above and enabling better collaboration and sharing of information and expertise (between academics, OH providers and employers). This proposal is particularly important to OH providers and the academic community.
Suggestions for improving the infrastructure included providing a mechanism for networking and keeping the sector up-to-date with the latest OH developments, ensuring research funding is targeted towards key evidence gaps and improving dissemination of research to support best practice in the Occupational Health sector.
The responses and suggestions for improvements in this area echo findings from recent government research with OH providers. The study suggested OH providers may benefit from access to structures that support the innovation process. For example: information and evidence on the benefits of investing in innovation to help providers overcome perceived financial risks; access to information that helps providers evaluate the impact of their innovations; clarity on and access to the most up-to-date, high-quality research that can inform service development and help providers easily maintain their knowledge with the latest OH developments; and opportunities to collaborate/network with others in the market to drive innovations.[footnote 66]
What government intends to do next
Government is committed to working with the market and key stakeholder organisations to explore how it may be able to support innovative ideas that increase the purchasing of OH by SMEs and the self-employed.
Government acknowledges the need for innovation that prioritises new OH service models and ideas that make greater use of technology. The responses show there is potential for government to support more rapid innovation in these areas; however, more intelligence is needed to understand precisely what role government can play and how any new innovation can add value to the innovation already happening in the market, particularly in light of COVID-19.
Government will gather this intelligence through targeted market engagement which will help inform policy proposals to support innovation in OH. We will continue to monitor emerging evidence from the COVID-19 emergency, to understand the extent to which the market has been driven to adopt new approaches in response to the pandemic, and how government can best support future efforts in the innovation space.
Government acknowledges widespread support for a new model to improve the prioritisation, co-ordination and dissemination of working age health research, both from the consultation responses and ongoing engagement with the OH community. Government also recognises how a new model could address some of the challenges to innovation identified in the research cited above.
In response, government has established a collaborative partnership with the Economic and Social Research Council (ESRC), the Medical Research Council (MRC), the Health and Safety Executive (HSE), the Society of Occupational Medicine (SOM) and the independent Academic Forum for Health and Work to develop the proposal for a new Centre for Work and Health Research. Government is committed to further developing the proposal with these delivery partners, including exploring the merits in the form of a potential new centre by beginning development work in this area starting this year.
This work will take account of stakeholders developing other relevant interventions in this area, including the National Institute for Health Research’s (NIHR) new Policy Research Programme for Working Age Health (NIHR PRP). This valuable new programme of research represents a significant investment by NIHR. The programme will fund a number of studies focusing on long-term, strategic policy issues in relation to work and health. The studies will generate new evidence and insight that can be used by government to inform its future strategy and policymaking.
Workforce
Longer term, there is widespread concern over shortages within the OH workforce, particularly of clinical staff. Combined with relatively small amounts of spare OH provider capacity, this risks limiting the market’s ability to deliver services in the future, as 44% of OH providers report having roles (typically, OH nurses and OH doctors) that they are unable to fill.[footnote 67]
In order to support current capacity and respond to increased demand, government aims to:
- address shortages within the OH workforce, ensuring the right training and support helps build a sustainable workforce for the future
- work towards building a sufficient supply within the market for new or existing OH providers to service future demand
- reduce the public purse burden through an improved commercial market partnership
Respondents were supportive of all OH workforce proposals, offering diverse feedback and constructive suggestions as to how proposals could be developed further.
Workforce intelligence
There was strong support for better OH workforce intelligence including some respondents suggesting submitting such data should be mandatory. The majority of OH providers agreed that they would be willing to submit information about the make-up of their workforce to a coordinating body. Whilst in favour of building a picture of the OH workforce which captures a wide range of roles and skill sets, respondents highlighted data protection as a key consideration. Others felt it may be too administratively onerous for smaller organisations and raised concerns that an appointed coordinating body may not be representative of smaller organisations or multidisciplinary teams.
Clinical expansion
The consultation sought views on improvements within the OH clinical workforce. Responses reflected the decline in workforce numbers and supported government intervention intended to build capacity within the OH workforce. In order to improve uptake and to ensure the sustainability of the profession, respondents outlined a wide spectrum of ideas, ranging from greater promotion of the profession to financial investment of training places.
Respondents felt greater promotion of the specialism and availability of dedicated OH courses is required, which needs to be driven by faculties and higher education institutions (HEIs). Alongside this, respondents highlighted the need to improve recruitment models into training, as current processes were felt to be too bureaucratic.
Further suggestions to improve capacity on a slightly larger scale include creating additional routes into the specialism, through core, cross-cutting training within clinical programmes, aiding greater transfer into OH. Responses also highlighted that current OH NHS training programmes do not always meet the needs of the commercial sector, making it difficult for the public and private sector to utilise OH specialists more effectively and enable further expansion opportunities.
Funding was a common theme in the responses received, with some respondents suggesting that more investment is required into the profession. Respondents said that a collaborative approach between the public and commercial sector was needed in relation to investment. It was also felt that better support through qualified trainers and supervisors is needed for clinical training, development and accreditation of OH professionals, helping to maximise workforce retention.
Multidisciplinary workforce models
There were a number of common themes noted in the responses received focusing on multidisciplinary and clinical expansion proposals, including training and financial support and the development of dedicated OH programmes. This suggests that integration of clinical and multidisciplinary solutions could benefit the OH profession overall.
Responses said that moving towards a biopsychosocial model which is multi professional would help support the sustainability of the future OH workforce and enable cost-effective OH service provision. Respondents highlighted that such an approach would help: properly utilise a wider range of skills, support clinical pressures, create greater access to OH services and support continuous professional development. It was acknowledged that in order to start utilising such skills, greater recognition of what other healthcare professionals, who are not OH doctors or OH nurses, could bring to the OH profession was required, which also included allowing greater flexibility for those wanting to transfer into the specialism.
Respondents told us there should be greater access to training placements for a wider range of trainee specialists, including greater collaborative training opportunities between the public and private sectors and commercial providers, helping maximise skills and experience. Some responses said that OH training programmes needed updating. Government acknowledges the suggestions made to support healthcare professionals to move towards a multidisciplinary approach and advise organisations on effective OH service delivery.
Respondents felt that to move towards a multidisciplinary approach, more financial support would be needed to support the diverse range of existing and trainee non-clinical healthcare professionals wanting to specialise or further support the OH profession. Responses also said financial support is needed to support the introduction of technology and information networks as potential routes to supporting cost-effective multidisciplinary service delivery models. It was expressed that development in such areas would support the dissemination of OH information and raise the profile of the specialism.
Leadership
Respondents said there is a need for a single body to lead on a range of OH workforce related issues, such as strategic workforce planning, training and development, governance, workforce models and standard setting. Respondents have suggested that the single body should be representative of a multi-disciplinary OH workforce and that representation should come from the range of clinical and non-clinical OH disciplines and healthcare professionals, recognising the role each professional group plays in the delivery of OH services.
What government intends to do next
Government recognises the need to build a better picture of the OH workforce which supports effective strategic workforce planning. Steps are being taken to understand how this can be achieved through digital data sharing, through the initiation of a discovery project. The potential benefits of an OH workforce digital data collation service are currently being explored, with outputs leading to an improved understanding of a potential digital solution. Government is currently collaborating with expert OH stakeholders from the public and commercial sectors to progress this work and determine next steps following this discovery phase.
Government is committed to supporting a sustainable OH workforce, recognising that immediate actions are required, alongside the development of a longer-term strategy, which acknowledges the cultural, behavioural and administrative changes required amongst organisations and stakeholders. Government recognises that this is a large programme of work and will initially focus on immediate actions around the provision of information and advice for OH professionals and those interested in an OH career, alongside exploring training improvements and support. These actions will help inform the longer-term workforce strategy which could include creating greater training and development opportunities for the current and future workforce subject to future funding. Government has initiated steps involving collaboration with expert OH stakeholders from the public and commercial sectors to develop these initiatives, as well as considering how the strategy could align with other programmes of work across government, with potential to collaborate in certain areas.
Government understands the importance of multidisciplinary working in OH and is therefore taking steps to understand the importance of involving a wide range of disciplines and healthcare professionals across public and commercial sectors in supporting the sustainability of the future OH workforce. Government has initiated research to expand the limited evidence base around multidisciplinary OH workforce models and are working with partners to understand uptake of this approach, including barriers, enablers and effectiveness, alongside impacts in light of COVID-19.
Government recognises the OH specialism requires an OH leadership function to support expansion, development and maintenance of a sustainable workforce. Government has started working with internal and external stakeholders to understand and identify what the function and specific requirements might be, where it could be hosted and how government might support this activity.
Chapter 5: Other issues raised in the consultation
The package of measures proposed forms just one part of the wider work and health system. In submitting responses some respondents drew on the broader work and health context, highlighting other important issues for government to consider. The most relevant of these are explored in more detail below.
Enabling better use of the fit note
The government wants employers and employees to have more productive conversations about work and health to support employee retention. This is even more important in light of COVID-19, with the relationship between work and health more prominent than ever before.
Although not specifically consulted on in ‘Health is everyone’s business’, many respondents took the opportunity to highlight the importance of the role of the fit note and how government can ensure it is used more effectively in future. Employers expressed their views regarding the use of fit notes during the consultation in relation to the provision of SSP. Two examples stated:
Fit Notes associated with the statutory sick pay system are not working and fail to provide specific advice or feedback for employers. This can frustrate more effective returns to work
Appropriate HCPs or Employment Advisers in primary care surgeries should provide the fit note and not the GP, given GPs cannot be expected to know the impact of each condition
Government is committed to improving the fit note to enhance work and health conversations and the support provided to both individuals and employers. While there has been some progress, for example the publication of ‘Talking Work’ guidance for GPs, which includes clinical guidelines for workplace adjustments for the top five clinical reasons people are off work sick or are on health-related benefits, and development of training for healthcare professionals, there is more to do.
What government intends to do next
Government has learned valuable lessons from COVID-19. Employers have responded positively and demonstrated flexibility during these difficult times, using alternative evidence such as the Isolation Note to support the payment of SSP.[footnote 68] General Practice has increasingly moved to a virtual consultation model, driving demand for a digital solution to the provision of fit notes. Learning from this, in the context of a transforming primary and secondary care landscape that is increasingly delivering care through a multi-disciplinary workforce, and the changes proposed earlier in this document for OH, government wants to ensure the fit note can be delivered in a way that facilitates good work and health conversations supporting workplace adjustments or return to work conversations with employers. Government will be taking the following action to ensure the fit note is transformed for the future:
- supporting the digital agenda post-COVID-19 by transforming the provision of medical evidence, including:
- ongoing support for the Isolation Note 111 Service by working cross-government to continually monitor and review the service and to update it in line with changes to public health guidance on self-isolation
- delivering further digital transformation including updating how fit notes are certified (to remove the current requirement for them to be signed in ink)
- creating a new interactive version of the fit note which will provide advice and support for suggested workplace adaptations or modifications, based on clinical conditions, to encourage work and health discussions between patients and employers
- exploring the amendment of regulations to allow a wider range of eligible healthcare professionals to sign fit notes
- commissioning Health Education England to develop an e-learning training module (summer 2021) to support eligible healthcare professionals with providing fit notes once they are permitted to do so
- promoting the use of Allied Health Professionals Fitness for Work Reports as an alternative to fit note, where appropriate to ensure the appropriate healthcare professional supports work and health conversations including for workplace adjustments or return to work conversations with employers
- embedding electronic fit notes in hospital systems and encouraging hospital doctors to issue fit notes to patients in their care, reducing the burden on GPs in primary care (from spring 2022)
- consulting employers to explore their views regarding using fit notes as medical evidence and consider how the government can address employers’ concerns in further fit note reforms
The role of insurance
Some respondents highlighted the importance of insurance products such as Group Income Protection (GIP) and Individual Income Protection (IIP) as another way of supporting workers’ health and wellbeing. There are a range of policy types available. GIP insurance products offer one way for employers of all sizes to access a range of expert-led support should it be required, such as counselling services, OH or vocational rehabilitation, as well as the provision of income in the event of sickness absence. The government agrees that, where policies are accompanied by high-quality services aimed at preventing ill health and offering support to return an employee to work, insurance products are a valuable source of support, in addition to offering a financial benefit if an employee is unable to work due to illness or injury. Some IIPs can provide similar benefits for the self-employed.
While insurance products might not be appropriate for some employers, as noted in ‘Improving Lives: The Future of Work, Health and Disability’[footnote 69], the government recognises the positive work across the industry to advance the offer for employers, particularly SMEs, such as developments in the provision of digital services.
What government intends to do next
Government welcomes recent proposals from the industry body Group Risk Development (GRiD) to develop a ‘consensus statement’ which aims to enhance employer guidance in partnership with business organisations and employer networks to improve employers’ awareness of the link between good work and good health, and to promote the use of expert-led support services to prevent and effectively manage sickness absence.
Government will support the creation of the consensus statement for employers and consider the outputs of the working group. The government will also continue to work with the industry to improve awareness among employers and self-employed people of the benefits protection policies can provide.
Tax
Several larger organisations called for tax incentives, linking to an earlier campaign to better incentivise employers to invest in health and wellbeing for staff. The incentives suggested by these larger organisations included treating OH-recommended treatments as a non-taxable Benefit in Kind. However, this suggestion was not reflected in responses from SMEs. The stakeholders that suggested the consideration of tax incentives referred to evidence on ‘blue collar’ workforce access to OH services, where disparities also exist.
Employers are already able to provide a number of health and wellbeing initiatives for their employees which are tax and National Insurance Contributions (NIC) exempt and not treated as a taxable Benefit in Kind. This includes up to £500 towards recommended medical treatments to help employees return to work, eye tests, and an annual health check. Employers can also create their own in-house facilities, such as gyms, or provide free onsite meals for employees without incurring NICs or tax.
What government intends to do next
The government does not believe that making the tax treatment of health and wellbeing initiatives more generous is the most effective way to incentivise employers to take positive action for their employees’ health and increase the provision of OH support. In part this is because there are often other barriers for employers in providing OH services, including the upfront costs. In addition, further tax relief would provide a greater benefit to those paying higher rates of tax and would not benefit individuals with income below the personal allowance. However, in response to feedback provided through the consultation and in recognition that the availability of welfare counselling is variable, changes were made in the March 2020 Budget to enable employers to provide non-taxable counselling services including any recommended related medical treatment such as cognitive behavioural therapy. The changes took effect from April 2020.
Access to Work
A number of responses commented on the valuable contribution Access to Work makes in supporting disabled people and those with long-term health conditions to receive adjustments to enter into and remain in employment, and thought more could be done to promote the service among employers and individuals.
What government intends to do next
The government continues to promote Access to Work as part of Disability Confident, including via a mailshot to all disability confident employers. Government is also undertaking further marketing and promotion of the Access to Work programme. This includes working with stakeholders, partners and employer associations to raise awareness through communications to their customers, and ensuring advisers who work with potential customers, including Jobcentre Plus, health professionals and advisory groups, have the information and tools to act as advocates.
In January 2021 the government launched a communication campaign to increase awareness and widen the reach of Access to Work. Alongside the campaign, pro-active press engagement activities were delivered to demonstrate the value of Access to Work and highlight positive case studies.
Government recognises the need to raise awareness of Access to Work with young disabled people, to join up adjustment support and improve the transition from education into employment. DWP is working with the Department for Education to pilot a new Access to Work Adjustments Passport. The Adjustments Passport will highlight the support available from Access to Work and capture adjustments or support needs already identified, to speed up the Access to Work customer journey and reduce the need for holistic assessments. DWP will also pilot the Adjustments Passport with veterans leaving the armed forces, and freelancers and contractors moving between job roles.
Additionally, the Health and Disability Green Paper explores the role of early intervention in back-to-work support, ensuring jobcentres are welcoming, engaging and expert and the importance of tailoring employment support to the needs of the individual.
Conclusion and next steps
Overall, government has heard there is a strong case to deliver the package of measures outlined in ‘Health is everyone’s business’, in order to reduce ill health-related job loss and support employee retention.
In light of COVID-19, and the need to protect and maintain progress made in disability employment, as well as boost the economic recovery, this aim is more important than ever before.
Government is committed to delivering the consultation package and to working closely with employers and their employees to ensure its success.
Consultation responses have informed crucial modifications to the proposals. These modifications will ensure the package strikes the right balance between increases in employer responsibilities and enhanced government support, with the capability for proposals to evolve with the benefit of learning from the pandemic.
The pandemic has highlighted the crucial links between work and health, as well as the potential of collaboration between employers, employees and government to tackle significant new challenges.
Ongoing collaboration to deliver the proposals set out in this response will put us in a strong position to continue working constructively together to meet the challenges ahead. This will reduce the chance that certain individuals or groups are left behind.
The package will ensure all employers are equipped to do the right thing for their employees, particularly helping disabled people and people with health conditions stay in and thrive in the new world of work.
Government will continue working with key stakeholder organisations, employers and employees to deliver the proposals. We will also continue to work with the Cabinet Office Disability Unit to align with the National Disability Strategy, which is also due to be published in 2021.
In summary, government will proceed with measures to help employers better navigate the work and health system, including enhancing resources to support COVID-19 returns to work/workplaces and developing a national information and advice service for health, work and disability (Chapter 1). Government will not proceed with a new right to request work(place) modification, but will consider measures to raise awareness and understanding around existing rights and responsibilities under the Equality Act 2010. Government has asked HSE to develop non-statutory guidance to support disabled people and people with long-term health conditions to remain in work and on managing any related sickness absence. They will also explore introducing statutory guidance in this area (Chapter 2).
The consultation posed several important questions on the future of SSP which require further consideration. Government maintains that SSP provides an important link between the employee and employer but that now is not the right time to introduce changes to the sick pay system
Finally, government will proceed with its strategy to reform the OH market and improve employer access to high-quality OH support by testing a potential new OH subsidy; exploring how government can support the development of innovative OH services; exploring the merits and form of a potential new Centre for Work and Health Research to support continuous research and development; providing access to buying support that can help employers purchase high-quality services; exploring the potential of outcome-linked measures in supporting providers to improve and innovate and help employers to choose the most appropriate services for their needs; and addressing capacity issues in the OH workforce (Chapter 4).
Annex
A. Costs and benefits: overview and methodology
This overview aims to indicate the potential scale of the impacts of the ‘Health is everyone’s business’ policy package and sets out the methodology behind the measured impacts. This annex covers the following areas: an introduction (section 1), benefits (section 2), costs (section 3) and monitoring and evaluation (section 4).
1. Introduction
The 2019 ‘Health is everyone’s business’ consultation set out policy options to help employers manage sickness absence and reduce health-related job loss. The government has responded, providing an overview of the responses received and details of what the government intends to do next to take forward the package of measures (this is set out in more detail in the main response).[footnote 70] They cover the following policy areas:
- Information and Advice (Chapter 1)
- New Guidance (Chapter 2)
- Statutory Sick Pay (SSP) (Chapter 3)
- Occupational Health (Chapter 4)
This overview outlines the potential impact of the policy package confirmed in the consultation response. It does not include policy proposals that are being kept under review.
We anticipate that the policies confirmed in the response will be most effective as a package, as taking forward some elements of the package in isolation might not have the desired impact. This is because the policies are complementary and are likely to be more effective if implemented together. For example, the improved information and advice service and new guidance is likely to encourage demand for Occupational Health (OH) services. This increase in demand will need to be met with a boost to OH services market capacity. The cumulative benefit of this could be increased support and retention of disabled people and people affected by ill-health. Therefore, this annex sets out the estimated costs and benefits of individual policies and then places them in the context of implementing the policy package.
The consultation response sets out a balanced package of measures which may bring costs to employers. These arise from implementing the new guidance and the purchasing of OH services. However, these costs are minimal when considering the potential benefits to society, employers and individuals of reducing health-related job loss and sickness absence. These benefits are realised through reduced recruitment costs and productivity gains for employers. There is a large evidence base that suggests unemployment causes worse physical and mental health outcomes for individuals. Additionally, the policy proposals will encourage employers to adopt workplace interventions, such as better sickness absence management. The evidence strongly suggests that this will reduce sickness absence, which has the potential to reduce costs for employers and employees significantly.[footnote 71] Finally, an improved information and advice service, new guidance and use of OH services will particularly benefit small and medium sized business (SMEs), who are less likely to provide formal support to employees with ill health and may lack the time, capacity or expertise to manage health events in the workplace.[footnote 72]
2. Benefits
2.1 Monetised benefits
Benefits to employers
The policy package gives employers easily accessible information and support to manage employees with health conditions, which they can choose whether or not to adopt. Utilised effectively, this package is expected to reduce health-related job loss, which the estimates below suggest could save employers between £5,000 and £11,000, on average, for each employee they prevent from falling out of work (subject to the caveats detailed). This results from the monetised productivity benefits of an individual remaining in their current role and replacement costs avoided by preventing a new vacancy. Details of the methodology are provided below.
Caveats
Much of the underpinning data used to inform the parameters of the estimates provided below come from a single study of the business costs associated with turnover from 2014.[footnote 73]
Whilst the study did include some diversity of business sector and size, the overall sample was relatively small (around 500 employers) and limited to only five main sectors (Retail, IT and Technology, Legal, Accounting, and Media and Advertising).
The focus of the study was on employees earning at least £25,000, which means that the data reported are biased towards those on higher incomes. The likely effect of this is to bias the average estimates upwards.
The majority of the figures reported in the study are self-reported and, therefore, subjective estimates, as opposed to objective data provided directly by management information. Notwithstanding the fact that the study only considers employees earning at least £25,000, the estimates provided are an attempt to give a sense of scale of the average benefits of retention and the specific components these are composed of. Clearly there will be huge variation in the actual benefits that would accrue to any individual business – this will be determined by many factors, for example: type of post, skill level, experience required, ease of replacement, local supply-side factors.
I. Productivity benefits to the employer (average)
The monetised productivity benefits account for the period of time it takes a new hire to become as productive as the member of staff they replaced. Businesses benefit from avoiding this productivity loss by retaining an employee.
Table 1: Productivity (£)
| Parameter | Description | Lower | Median | Upper |
|---|---|---|---|---|
| Average number of weeks of lost productivity associated with new hires | Taken from ‘The Cost of Brain Drain’ paper from Oxford Economics (2014)[footnote 74]. The study surveyed 500 firms of various sizes across five sectors on how long they estimated it took an individual to reach optimal productivity, based on where they had been recruited from and the size of the firm.[footnote 75] These estimates of the path to optimum productivity are used to calculate an estimate for the average number of weeks of lost productivity in total per employee replaced.[footnote 76] The figures reported here show the range of firms’ responses across all sectors and sizes associated with recruiting somebody from the same sector with some experience. Figures are generally higher if considering recruitment from another sector, without experience or someone that has been unemployed/inactive for a period of time. |
3.8 | 6.4 | 8.0 |
| Average weekly gross pay (median) | Taken from the latest ONS Annual Survey of Household Earnings figures (2019 revised) for all employees in the UK[footnote 77]. This is used as proxy for productivity. | £500 | £500 | £500 |
| Productivity | Product of time and wage. | £1,800 | £3,100 | £3,800 |
Note: figures have been rounded.
II. Replacement costs avoided by the employer (average)
Replacement costs consist of advertising and agency fees, cost of temporary cover, cost of HR process and the cost of interviewing, which all relate to the recruitment of an individual into post once an employee falls out of work. These aspects are all summed to give a range for the overall average of replacement costs per vacancy. The estimates below are largely calculated using data from Oxford Economics (2014) unless otherwise stated.[footnote 78]
Table 2: Replacement costs (£)
| Parameter | Description | Lower | Median | Upper |
|---|---|---|---|---|
| Average spend on advertising and agency fees | Using the paper’s survey data, we multiplied the proportion of firms using these respective services by average costs across reported sectors and firm sizes to determine a range of average spend on advertising and agency fees per vacancy. | £200 | £500 | £900 |
| Average spend on temporary cover | Based on the assumption that firms use a temporary worker for an average of 18 days per vacancy. The range of average costs reported here is taken directly from the range of values reported in the paper as official national data for temporary cover is not available. |
£2,000 | £3,500 | £5,000 |
| Average HR process costs | The paper reports an average time used per vacancy of between 1.5 and 2 HR person-days. We take this range and multiply it by the latest median ONS Annual Survey of Household Earnings figure for the ‘Human resources and industrial relations officers’ occupational class.[footnote 79][footnote 80] |
£200 | £200 | £200 |
| Average costs of interviewing | The paper reports an average cost of interviewing per vacancy of around £700–800 across the sectors and firm sizes surveyed. This is based on 2–3 director-level staff each spending around one hour on preparation and one hour on interviewing. The paper reports that the study found little variation by firm size in the number of candidate interviews per vacancy. The majority of variation in interview costs reported is associated with variations in average salary rates for the director-level staff across sectors. The range of average interviewing costs reported here is taken directly from values reported in the paper across the five sectors sampled. |
|||
| £500 | £800 | £1,000 | ||
| Replacement costs | Sum of the above cost categories. | £2,900 | £5,000 | £7,100 |
Note: figures have been rounded.
These estimates assume substitution, that is to say an individual not retained by their employer would be replaced by somebody from within the same sector. [footnote 81]
Table 3: Societal benefits of retaining an individual in work (£)
| Employer benefits | Lower | Median | Upper |
|---|---|---|---|
| Productivity | £1,800 | £3,100 | £3,800 |
| Replacement costs | £2,900 | £5,000 | £7,100 |
| Total | £4,700 | £8,000 | £11,000 |
Note: Figures have been rounded.
Benefits to small businesses
SMEs are the focus of a number of the policy proposals because evidence indicates that they are generally less likely to provide formal support to prevent employee ill-health or improve general wellbeing. Therefore, they are less likely to be active in supporting employees to remain in work.[footnote 82]
The information and advice proposal offers easily accessible and better integrated health and disability-related information for employers over the internet, through gov.uk, which is designed with the needs of SMEs in mind. SMEs with at least one employee (1–249 employees) make up 99% of all businesses in the UK. Additionally, approximately half of small employers use the internet as their main source of support information, compared with a quarter of large employers.[footnote 83] This highlights the potential scale of the impacts of these policy proposals.
Small businesses are also less likely than large businesses to have a dedicated HR team and there are lower retention rates for disabled employees in small workplaces than in large workplaces.[footnote 84][footnote 85] Through this policy package, better and more targeted support is expected to benefit small businesses in particular, for example, if they take the OH subsidy and an employee has reduced sickness absence or is prevented from falling out of work.
Benefits to individuals
The policy package can also have long-term mental and physical health benefits for individuals if utilised effectively. Increasing support to manage sickness absence and health conditions is expected to reduce long-term absences from work and prevent individuals with health conditions from falling out of work.
There is a large and established literature that demonstrates an association between unemployment and negative health outcomes. Long-term unemployment is consistently associated with poor physical and mental health, higher mortality and greater use of health resources. This association is seen across the age spectrum and in both sexes and is not accounted for by the social-class distribution of the unemployed.[footnote 86]
However, there is no currently available evidence to support a detailed, robust estimation of the dynamic impact of a loss of employment on health outcomes that would enable monetisation. Detailed cohort analysis of both work and health outcomes is required to support comprehensive estimates of the health benefits of retention.
Public Health England have a published ‘Movement into employment: return on investment’ tool that supports estimation of the benefits of moving an individual from unemployment into stable employment.[footnote 87]
The monetised potential health benefits figures set out below, taken from the PHE tool, represent the average potential health benefits of moving from unemployment or inactivity into stable employment for at least one year. These are estimated to be between £1,700 and £6,400, which offers a sense of scale regarding the impact of a change in employment status on health.
PHE’s methodology is set out as follows:
Table 4: Individual health benefits of movement into stable employment from unemployment
| Parameter | Description | Lower | Median | Upper | |
|---|---|---|---|---|---|
| Quality Adjusted Life Years (QALY) change (per person moving into stable employment from unemployment or inactivity)[footnote 88] | Public Health England’s Movement into Employment: Return on Investment tool considers the impacts of individuals moving from unemployment to stable employment.[footnote 89] | It considers the difference in health state for an individual that moves between unemployment and at least one year of stable employment, using changes in SF-36 health domain outcomes to produce a change in terms of QALYs.[footnote 90] The range reported here uses the standard errors reported alongside the central estimates for each of the eight SF-36 domain values to generate confidence intervals for each, at the 95% level, which are then used to derive a range overall.[footnote 91] |
0.0282 | 0.0675 | 0.1068 |
| Monetary value of a QALY | The National Institute for Health and Care Excellence’s monetary value per QALY | £60,000 | £60,000 | £60,000 | |
| Individual health benefits | Product of change in QALY and monetary value of QALY | £1,700 | £4,100 | £6,400 |
It should be noted that whilst the studies used to inform the development of the PHE model use all eight domains of the SF-36 questionnaire (general health, physical functioning, bodily pain, mental health, vitality, social functioning, role functioning – physical, role functioning – emotional), the focus of those studies was on mental health impacts. Physical health impacts were seen as a secondary issue and the authors acknowledge a scarcity of evidence around physical health impacts in the literature.
The SF-36 questionnaire used in the studies has been validated psychologically but it is not diagnostic with respect to health conditions. Therefore, strictly speaking, the impacts referenced are perceived health impacts inferred from self-reported scores.
2.2 Non-monetised benefits
There are benefits from the policy package which cannot be monetised at this point as it requires policy implementation and evaluation data.
Actions that support workers with sickness absence to return to work will generally reduce the number of sickness absence days taken. The policy proposals are designed to encourage greater take-up of workplace interventions. Existing systematic reviews of work and health intervention studies conclude that there is good quality evidence that workplace interventions are effective in reducing work disability duration, i.e. time spent out of work due to ill-health.[footnote 92] These are nearly always multi-component interventions and include early contact and sustained support by the workplace, work accommodations and coordination between health care and the workplace.
Additionally, OH services are an important enabler of these best-practice workplace interventions. Research internationally has highlighted their role in identifying and implementing effective return to work arrangements and workplace accommodations, in mediating the interactive process between employer and employee, and the benefits of OH services over GP advice in rehabilitation through knowledge of and connection with workplaces.[footnote 93]
This evidence shows that supporting workers to return to work will generally reduce sickness absence, and earlier returns to work reduce the cost to employers of lost productivity and sick pay. However, it is difficult to quantify what this impact would be as there is no measure of the ‘right’ level of sickness absence, i.e. the sickness absence duration that enables the employee to recover properly and return to work with support. A good way to measure this could be less sickness absence over time and a proxy of this could be the speed of return to work.
Managers will benefit from the new guidance and information and advice service, as it is expected to build their confidence in supporting staff.[footnote 94] Increased clarity and information from this may lead to better sickness absence management, which can prevent long-term sickness absence costs for the business. It is also expected to have direct benefits for small employers who are less likely than large employers to have a specific policy in place to manage sickness absence.[footnote 95] There will also be cost and time savings for employers who have cited lack of time and staff resources as a barrier to providing support.[footnote 96]
The OH policy package is expected to serve as a means through which employers can carry out recommendations, outlined in the new guidance and information and advice service, to its full effect. Additionally, the development of products to improve the process of choosing quality and cost-effective OH is estimated to be a cost saving for employers as it will reduce the time they spend on acquiring effective information.
2.3 Wider impacts, transfers and benefits
In addition to the benefits above, the policy package is also expected to have some wider impacts and transfers.
Cost is a barrier to purchasing OH, particularly for SMEs and the self-employed. The OH subsidy test will enable SMEs and self-employed people to purchase OH assessments at a subsidised cost. A time-limited subsidy could also potentially lead to a long-term increase in OH demand. This will enable businesses to get expert advice on the best course of action to take when dealing with a complex sickness absence.
We also expect the new guidance and the information and advice service to have long-term qualitative benefits for society by standardising employers’ behaviour towards sickness absence. This in turn is expected to promote fairness and equality and can benefit employees who feel more vulnerable to job loss due to their disability, health condition or ethnicity.
The OH workforce expansion and market reform policies can be the means through which increased demand for OH is met in the market. The government is exploring the merits of and form of a potential new Centre for Work and Health Research. This could be cost saving for OH providers and employers in the long run by providing access to the latest research that could be used to develop more efficient ways of delivering OH services.
3. Costs
3.1 Monetised costs
Initially, the policy package will be updating existing non-statutory guidance around managing sickness absence, with a longer-term strategy of exploring the introduction of new statutory guidance. These costings currently relate to the new non-statutory guidance, which may lead to additional costs for employers. However, the voluntary nature of the policies initially mean that costs would only be incurred by those employers who decide to familiarise themselves with the new non-statutory guidance and adopt the recommended proposal of implementing return to work (RTW) plans for employees following long-term sickness absence (LTSA).
One-off business familiarisation costs
Businesses that are employers are expected to incur a one-off familiarisation cost in the first year of the new non-statutory guidance. This is estimated with the assumption that all medium and large employers (more than 50 employees) will read the new non-statutory guidance as a matter of routine, as they keep up with changing guidelines.
We anticipate that small employers (fewer than 50 employees) are less likely to incur familiarisation costs, as we assume they are unlikely to familiarise themselves with new non-statutory guidance until required.
Small employers are unlikely to have a dedicated HR team so a manager/director/senior official is more likely to manage sickness absence; this is captured under recurring costs.[footnote 97] Large employers are more likely to have an HR function so a corporate manager/director will manage this.
Table 5: One-off business familiarisation costs
New non-statutory guidance
| Time (hours) | Management cost per hour (£) | Number of businesses | Total business cost (£) | |
|---|---|---|---|---|
| Small (1–49 employees) | 0 | 31.29 | 1,368,770 | - |
| Medium (50–249 employees) | 2 | 33.39 | 36,140 | £2,414,000 |
| Large (250 or more employees) | 2 | 33.39 | 7,835 | £523,000 |
| Total | £2,937,000 |
To note: Figures have been rounded. Source: Wage rates are from Annual Survey of Household Earnings (ASHE) 2019 table 20.5a.[footnote 98] Wage rates have been uprated to account for non-wage labour costs, in line with corresponding ONS data on labour costs.[footnote 99] It is assumed to take 2 hours for businesses to familiarise themselves with new guidance. Total cost is calculated using business population estimates.[footnote 100]
In total we estimate that businesses will incur a one-off familiarisation cost of £2.9m in the first year of policy package implementation, given that all medium and large businesses familiarise themselves with the new non-statutory guidance. This cost is on average £67 per medium or large employer. This is calculated by dividing total business cost (£2.9m) by number of medium and large businesses (43,975).
Recurring better sickness absence management costs
We assume that the new non-statutory guidance will encourage employers to better manage employees on LTSA by developing, for example, RTW plans for them. However, better sickness absence management costs will vary depending on the exact non-statutory guidance the employers decide to implement. We assume small employers require more time to develop RTW plans, as no familiarisation time is being used, compared with medium and large employers. Additional time may also be needed in the event of seeking specialist advice.
These costs are based on management time required to set up RTW plans for employees on LTSA. However, employers who already do this will not accrue any additional costs from the new non-statutory guidance.
Table 6: Business sickness absence management cost
Volumes
| Number of businesses | Businesses without a RTW plan | LTSA in businesses without a RTW plan | |
|---|---|---|---|
| Small | 1,368,770 | 492,757 | 18,232 |
| Medium | 36,140 | 8,312 | 391 |
| Large | 7,835 | 392 | 21 |
| Total | 1,412,700 | 501,500 | 18,600 |
To note: Businesses without a RTW plan is (1-p) business population[footnote 101], where p is the proportion of businesses who develop a return to work plan for employees on LTSA. This is 64% for small, 77% for medium and 95% for large employers.[footnote 102] LTSA in businesses without a RTW plan is those without a RTW planproportion of business with likelihood of a LTSA.[footnote 103]
Cost
| Time (hours)* | Management cost per hour (£) | No. of LTSA in businesses without a RTW plan | Total business cost (£) | |
|---|---|---|---|---|
| Small | 5.5 | 31.29 | 18,232 | 3,137,600 |
| Medium | 5 | 33.39 | 391 | 65,200 |
| Large | 5 | 33.39 | 21 | 3,500 |
| Total | 18,600 | 3,206,300 |
*It is assumed to take 2 hours of management time to handle a sickness absence (for the conversation and any necessary actions) at the first intervention point (4-6 weeks). However, due to no familiarisation time being used by small employers, additional time may be needed in the event of a request to seek specialist advice and so an additional half an hour has been assumed here. At intervention point 2 (2-3 months), 2 hours of management time is assumed again, but without specialist seeking advice time for small employers as this is assumed to only be needed once. At post-sickness absence, an hour of management and employee time is assumed to cover multiple, brief conversations between the employee and their line manager about their return to work.
To note: Wage rates are from ASHE 2019 table 20.5a[footnote 104]. Wage rates have been uprated to account for non-wage labour costs, in line with corresponding ONS data on labour costs.[footnote 105] Total business cost is businesses in scope of adopting new guidance * cost per return to work plan.
We estimate that there will be approximately 18,600 LTSAs in businesses who do not currently develop a RTW plan for employees. If they adopt the new non-statutory guidance’s suggestion of developing one for each of these cases, the total additional better sickness absence management cost to all employers would be £3.2m every year. The cost for the employer is on average £172 per employee on LTSA. This is calculated by dividing total business cost (£3.2m) by number of LTSAs in businesses without a RTW plan (18,600).
In the longer term, introducing statutory guidance will be explored. The costs to business from this will depend on whether the businesses familiarised themselves with the non-statutory guidance and the similarity of the statutory guidance to the non-statutory guidance. This will determine the degree to which familiarisation will be required. Additionally, the incurred better sickness absence management costs due to the statutory guidance will depend on whether the businesses implemented RTW plans, as encouraged by the non-statutory guidance.
3.2 Non-monetised costs
The policy package promotes the use of OH services by making it easier for employers, in particular SMEs, to access services through improved processes of choosing OH, OH assessments subsidy test and general information and advice. Evidence shows that large employers are five times more likely to offer OH services to their employees than small employers.[footnote 106] Additionally, one in six employers cited cost as a reason for not providing access to OH, with knowledge of actual costs amongst small employers being limited.[footnote 107] Therefore, in combination with the rest of the package, the subsidy test is expected to generate demand for OH services. However, the purchase of OH services is entirely voluntary so additional business costs will vary depending on their current utilisation of services.
4. Monitoring and Evaluation
We are actively considering the appropriate scale and scope of our evaluation plans. We are considering the appropriate surveys we would require in addition to pre-existing national surveys (e.g. Labour Force Survey), relevant management information, and further research to capture the effects of the package and its elements. The Occupational Health subsidy test will have a full evaluation.
B. Interim summary: Discrete choice experiment exploring impact of incentives on SME uptake of health and wellbeing support schemes
Authors: Michael Oldridge, Lisa Schulze (DWP), Peter Burge, Hui Lu, Pamina Smith, Nadja Koch (RAND Europe)
Background
The ‘Health is everyone’s business’ consultation outlined the crucial role employers play in supporting the health of employees. Improved employee health and wellbeing can benefit employees, employers, and the wider economy by reducing ill-health related job loss, sickness absence, presenteeism, and improving productivity.
However, previous research shows that whilst most employers recognise their role, many face multiple barriers to investing in health and wellbeing support, such as lack of expertise, time constraints and cost. There is also wide variation in the support provided by employer size, with small and medium-sized employers significantly less likely to invest in formal health and wellbeing initiatives than large employers.[footnote 108]
The Department for Work and Pensions / Department of Health and Social Care (DWP/DHSC) joint Work and Health Unit commissioned RAND to research what incentives could be used to encourage and support SME employers to invest in more health and wellbeing schemes for employees.
Methodology
The research included a quantitative survey with 500 SME employers (with at least 10 employees) in Great Britain, 30 in-depth qualitative interviews, and a discrete choice modelling experiment embedded within the survey.
The survey and interviews explored the main health concerns of SME employers, their current provision of health and wellbeing support, and the barriers to providing it. The survey uses a sampling frame but is not weighted to be representative nationally.
The discrete choice experiment explored the potential impact of financial incentives and supplementary advice on SME take-up of health and wellbeing schemes, including the importance of attributes relating to how that support is delivered. Each SME was given a range of hypothetical ‘choice scenarios’. Within each scenario, SMEs were asked to choose between three options: two involving participation in a new health and wellbeing scheme and one ‘continue as now’ option. The health and wellbeing schemes offered were varied in carefully controlled ways by five groups of attributes:
| Attribute | Levels |
|---|---|
| Types of health and wellbeing services in scope for purchase | Proactive health-promotion schemes open to all employees, i.e. schemes to encourage healthy eating, or stress management Schemes targeted for employees with health conditions, i.e. occupational health assessments Both in scope |
| Needs assessment and advice on interventions | No support available – baseline Online resources available Personal adviser available |
| Financial support (% of cost is reimbursed) | No financial support – baseline 25% of cost is reimbursed 50% of cost is reimbursed 75% of cost is reimbursed 100% of cost is reimbursed |
| When support payment is made | All paid at the end – baseline 30% paid up front and 70% paid at the end |
| Administrative requirements | Only proof of purchase required – baseline Proof of purchase plus funding request submitted beforehand Proof of purchase plus requirement to provide data on impacts of scheme |
An example of a choice scenario put forward to respondents is below:
Choice 1 of 6. If offered the following options, which, if any, would your business choose?
| Option A | Option B | Continue as now | ||
|---|---|---|---|---|
| Type of schemes supported | Schemes open to all employees e.g. training and general support schemes | not supported | supported | |
| Type of schemes supported | Schemes for employees with known health conditions e.g. expert-led support and condition management | supported | supported | |
| Advice available | Needs assessment and advice on interventions | online resources available | no support | |
| Financial support | Amount reimbursed | 100% of cost is reiumbursed | 50% of cost is reiumbursed | |
| Financial support | When payment made | All paid at the end | 30% paid up front, 70% paid at the end | |
| Administrative requirements (proof of purchase plus) | You make a funding request beforehand | required | required | |
| Administrative requirements (proof of purchase plus) | You provide data on impacts of scheme | required | not required |
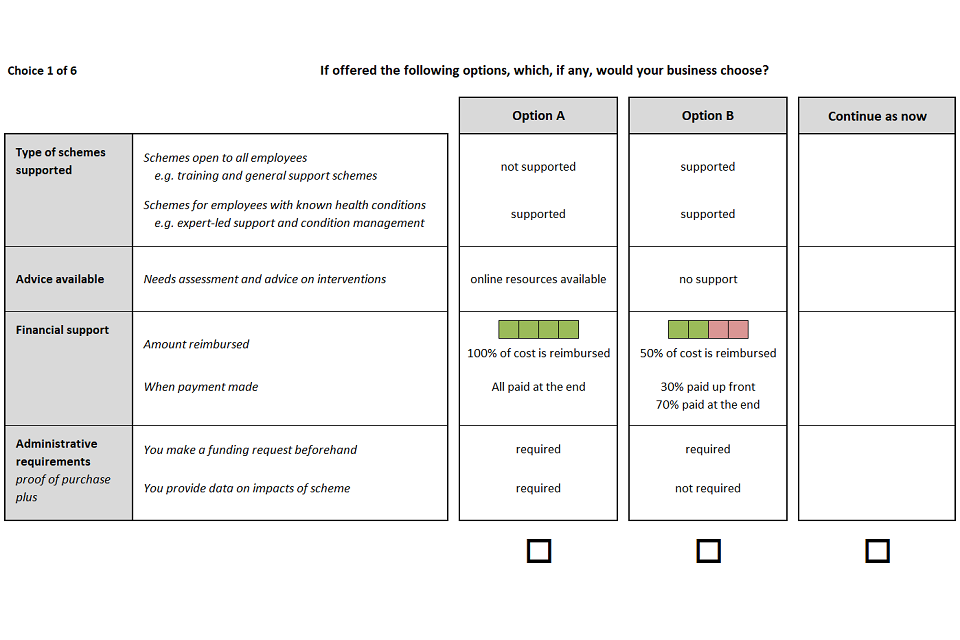
Responses were used to model the relative contribution of each attribute level to the likelihood that SMEs would choose a scheme. These were used to illustrate the potential SME take-up for schemes with different configurations of attributes. However, it is advised that specific take-up estimates should be interpreted with extreme caution for the following reasons:
- they assume 100% of SME employers are aware of any scheme. In reality, raising awareness of such provision amongst SMEs can be challenging
- the hypothetical scenarios did not include any detail on gross scheme costs. In reality, cost is likely to significantly influence employer take-up. It may also influence the relative importance of other factors, such as financial reimbursement rate
- responses may be subject to social desirability bias, meaning respondents may choose the more socially acceptable answer (that is, they would provide support) even if it’s not the choice they would make in reality
- the sample of respondents excluded micro employers (with fewer than 10 employees), who may be less likely to take up formal health and wellbeing support This research was carried out in 2018, prior to the COVID-19 pandemic.
Survey and qualitative interview findings
Key health concerns for employers
When asked about the most important health and wellbeing concerns affecting their organisation, over 80% of respondents reported each of musculoskeletal conditions or mental health problems. This supports previous research which found these to be the two most common health concerns of employers.[footnote 109] They are also the two single most common reasons for sickness absence in the UK after minor illnesses.[footnote 110]
The qualitative research highlighted that concerns about musculoskeletal conditions clustered into two different groups: those that were concerned about low levels of activity at desk-based work along with repetitive movements, and those that were concerned about heavy lifting and physical strain.
Concerns regarding mental health could also be clustered into two groups: those that were aware of the stresses and strains of the workplace, and those that recognised that their staff could have complications outside of work that could also impact on their working life.
Current provision of health and wellbeing support
Employers were asked about two categories of health and wellbeing scheme:
- proactive health promotion for all employees in the workplace – for example, schemes to encourage healthy eating, physical activity, or stress management
- support targeted for employees with long-term health conditions, beyond legal obligations – for example, OH assessments, or access to psychological therapy
70% of SMEs reported they currently provide at least one type of proactive health promotion scheme for all employees. This varied significantly by employer size, with only 58% of employers with 10–19 employees providing at least one type of proactive support, compared to 82% of employers with 50–249 employees. The most common types provided were mental health support or training (39%) and help with managing stress (39%).
Similarly, when asked about provision targeted for employees with health conditions, medium employers reported much higher levels of current provision. However, this is to be expected since smaller employers are less likely to have employees with health conditions. For example, previous research found that the most common reason small employers do not provide Occupational Health services for their employees was a lack of employee need.[footnote 111]
Therefore, to explore willingness to provide support, employers were asked both whether they currently provide support specifically for employees with health conditions, and whether they would provide it if an employee need arose. Taking into account this stated willingness to provide support should it be required, the difference by employer size reduces significantly, but a difference does remain.
Qualitative interviews highlighted that smaller employers did appear to have a strong interest in the health and wellbeing of their staff, but they tended to have more of a ‘family’ culture than larger employers and therefore tended to use more informal approaches to handling health problems in the workplace.
Figure 1: Targeted health and wellbeing schemes currently provided or would be provided to employees with health conditions, by employer size (n=500)
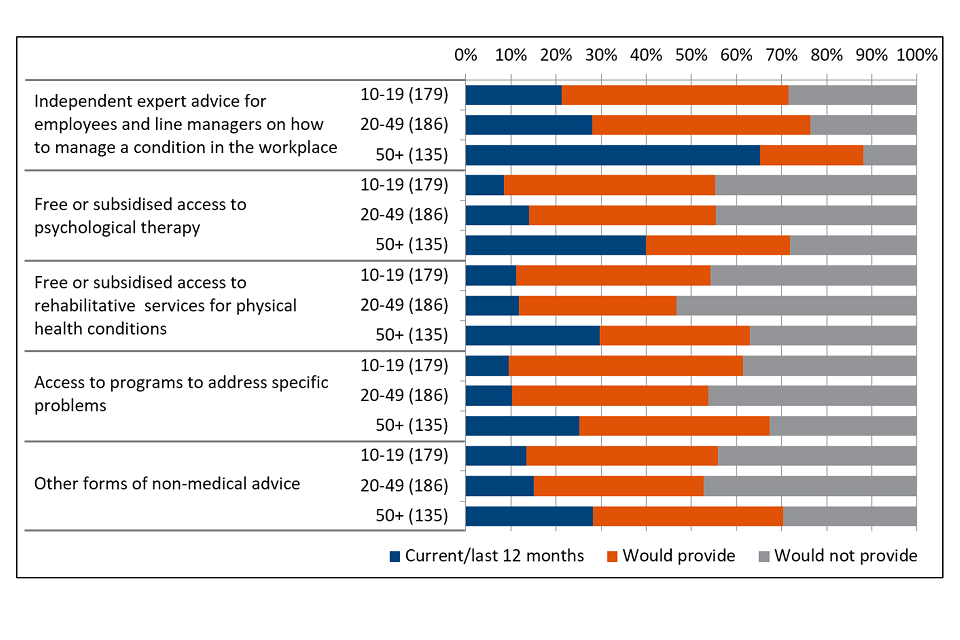
Independent expert advice for employees and line managers on how to manage a condition in the workplace
| Current/last 12 months | Would provide | Would not provide | |
|---|---|---|---|
| 10-19 (179) | 21% | 50% | 28% |
| 20-49 (186) | 28% | 48% | 24% |
| 50+ (135) | 65% | 23% | 12% |
Free or subsidised access to psychological therapy
| Current/last 12 months | Would provide | Would not provide | |
|---|---|---|---|
| 10-19 (179) | 8% | 47% | 45% |
| 20-49 (186) | 14% | 41% | 45% |
| 50+ (135) | 40% | 32% | 28% |
Free or subsidised access to rehabilitative services for physical health conditions
| Current/last 12 months | Would provide | Would not provide | |
|---|---|---|---|
| 10-19 (179) | 11% | 43% | 46% |
| 20-49 (186) | 12% | 35% | 53% |
| 50+ (135) | 30% | 33% | 37% |
Access to programs to address specific problems
| Current/last 12 months | Would provide | Would not provide | |
|---|---|---|---|
| 10-19 (179) | 10% | 52% | 39% |
| 20-49 (186) | 10% | 44% | 46% |
| 50+ (135) | 25% | 42% | 33% |
Other forms of non-medical advice
| Current/last 12 months | Would provide | Would not provide | |
|---|---|---|---|
| 10-19 (179) | 13% | 42% | 44% |
| 20-49 (186) | 15% | 38% | 47% |
| 50+ (135) | 28% | 42% | 30% |
Barriers to investing in health and wellbeing
The most common reported barriers to providing health and wellbeing support were lack of expertise to know what support to invest in (49% of respondents), lack of time or resources to implement policies (49%), and lack of capital (52%). This supports previous research which found that lack of time and capital are the main barriers for SMEs in supporting employees to return to work after a spell of sickness absence.[footnote 112]
A theme highlighted in the interviews was that knowing what to invest in is complicated and navigating the market can be difficult and requires a time investment. Some SMEs explained that whilst cost was a key barrier to SMEs, many would not know what health and wellbeing programmes to invest in even if there was financial support.
Discrete Choice Experiment findings
Importance of type of health and wellbeing scheme on SME take-up
SMEs were equally as likely to choose a preventative health and wellbeing scheme as they were to choose a scheme targeted for employees with health conditions, but they were more likely to choose a scheme including both types of support than just one.
SMEs with experience of employees with long-term health conditions or disabilities were more likely to choose either type of scheme than SMEs without that experience but they were particularly more likely to choose preventative schemes.
Importance of financial incentives on SME take-up, including payment timing
The experiment found that as the rate of financial reimbursement increases, the likelihood of choosing an option increases. However, there are diminishing marginal returns as reimbursement rates increase.
Taking the example of an option that covered both categories of health and wellbeing schemes, where 30% of any financial reimbursement is paid up front and 70% is paid at the end, which includes an online needs assessment and signposting to appropriate schemes, and for which there are no administrative requirements for participating, the experiment estimated that 53% of SMEs who know of the scheme would participate even if there was no reimbursement. If the government offered a 25% financial reimbursement, take-up would increase by 13%-points to 66%, but for each additional 25% reimbursement, the amount by which take-up would increase gets smaller. Increasing the subsidy to 50%, then to 75%, then to 100%, would increase take-up by a further 11%-points (to 77%), 5%-points (to 82%), and then 4%-points (to 86%), respectively.
In practice, this means that for a given pool of funding, greater impact could be achieved by funding a larger group of SMEs at 50% reimbursement than half as many SMEs at 100% reimbursement.
Table 1: Forecasts of take-up under different rates of reimbursement
| 0% | 25% | 50% | 75% | 100% | |
|---|---|---|---|---|---|
| Schemes open to all employees are supported Schemes targeted for employees with health conditions are not supported |
42% | 55% | 68% | 74% | 79% |
| Schemes open to all employees are not supported Schemes targeted for employees with health conditions are supported |
40% | 53% | 66% | 72% | 78% |
| Schemes open to all employees are supported Schemes targeted for employees with health conditions are supported |
53% | 66% | 77% | 82% | 86% |
To test whether capital, or more specifically cash-flow constraints, were the barrier for SMEs, the experiment varied the timing of the reimbursement payment between having a payment made on delivery, or having 30% paid up front and the remaining 70% on delivery. This had no statistically significant impact on take-up. This finding was generally supported through qualitative interviews, though some SMEs reported that a quick reimbursement following delivery was important.
It is worth noting however that information which was not provided in the hypothetical scenarios, such as gross scheme cost to providers, could change the relative importance of the financial reimbursement rate or timing of payment in reality.
This is particularly important given a common theme in the qualitative interviews was that many SMEs appeared to have limited understanding of the costs of health and wellbeing schemes, and many had not seriously considered how much they might be willing to spend. This means that many SMEs made decisions in the experiment without a clear and consistent understanding of the costs to the business.
Importance of supplementary advice and guidance on SME take-up
The choice experiment tested whether supplementary advice and guidance would increase take-up of a scheme. This was described as an upfront needs assessment to help SMEs better understand staff health needs or on how to source or implement best-practice schemes to address those needs. The experiment varied whether this advice was delivered through access to online resources or access to a personal adviser.
The provision of supplementary advice had a statistically significant positive impact on take-up of health and wellbeing schemes. However, on average there was no statistically significant difference between whether this support was delivered online or by a personal adviser. For example, Table 2 shows that by taking the same option as expressed in the previous section but holding the rate of financial reimbursement fixed at 50%, the availability of online resources or a personal adviser would increase SME take-up by 7–8 percentage points compared to if no advice was available.
Table 2: Forecasts of take-up of different levels of advice and guidance
| No advice available | Online resources available | Personal adviser available | |
|---|---|---|---|
| Schemes open to all employees are supported Schemes targeted for employees with health conditions are not supported |
60% | 68% | 69% |
| Schemes open to all employees are not supported Schemes targeted for employees with health conditions are supported |
58% | 66% | 67% |
| Schemes open to all employees are supported Schemes targeted for employees with health conditions are supported |
70% | 77% | 78% |
The qualitative interviews showed this represented a mix of preferences, with some employers strongly preferring online advice and others preferring a personal adviser.
Importance of administrative requirements on SME take-up
Including additional administrative requirements for employers to participate in a scheme had no statistically significant impact on the likelihood of employers choosing that scheme. However, in the qualitative interviews, many SMEs emphasised that any administrative requirements needed to be proportionate to the funding and support being provided. This indicates that whilst the experiment did not detect an impact, excessive and disproportionate administrative requirements could still have an impact on take-up.
Conclusion
Findings from the survey and qualitative interviews were consistent with other research. Medium-sized employers are more likely than small employers to invest in formal health and wellbeing initiatives for their employees. For support specifically to manage existing health conditions in the workplace, this difference by employer size reduces significantly when taking into account whether SMEs would be willing to provide the support should an employee need arise, yet a difference does remain. The most common barriers to SMEs providing health and wellbeing support were lack of expertise to identify initiatives, lack of time to implement, and lack of capital to invest in them.
The experiment, supported by qualitative evidence, suggests that the following could be effective at improving SME take-up of health and wellbeing schemes:
- financial support. However, a greater impact could be achieved by funding a larger group of SMEs at 50% reimbursement than half as many SMEs at 100%
- supplementary advice, in the form of a needs assessment and signposting to appropriate health and wellbeing schemes
-
DWP, ‘Shaping Future Support: the Health and Disability Green Paper’, July 2021. ↩
-
DWP/DHSC, ‘Improving lives: the future of work, health and disability’, November 2017. ↩
-
Only 44% of small employers (vs. 72% of large) are proactive in managing employee health and wellbeing. Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
DWP/DHSC Official Statistics. ‘The Employment of Disabled People - Data up to 2019’, March 2020. ↩
-
‘DWP COVID-19 Employer Pulse Survey Interim summary report’ DWP ad hoc RR78, July 2021. ↩
-
Working Families ‘COVID-19 and flexible working: the perspective from working parents and carers’ June 2020. ↩
-
McKinsey and Co ‘How COVID-19 has pushed companies over the technology tipping point—and transformed business forever’ October 2020. ↩
-
DWP/DHSC, ‘Improving lives: the future of work, health and disability’, November 2017. ↩
-
DWP, ‘Shaping Future Support: the Health and Disability Green Paper’, July 2021. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981, July 2021. ↩
-
IAPT is a service that provides evidence-based psychological therapies to people with anxiety disorders and depression. When Employment Advice is embedded in IAPT, therapists and Employment Advisers work with people to draw up plans to achieve employment goals. These plans will consider ways to improve mental health, support people to remain in work while receiving treatment, get back to work, if off sick, or to find work, if out of work. EA in IAPT is available in approximately 40% of IAPT services across England. It has provided support to 29,000 people in the 2020/21 financial year. ↩
-
ONS - A08: Labour market status of disabled people, July 2021. ↩
-
The disability employment rate gap has decreased by 5.3 percentage points between Q1 2014 and Q1 2021. ONS - A08: Labour market status of disabled people, July 2021. ↩
-
The government’s CJRS scheme had 2.4 million people furloughed in May 2021, down from a peak of 5.1 million in January 2021. Additionally, 11.6 million jobs have been supported by the CJRS since the start of the scheme. HMRC Official Statistics. ‘Coronavirus Job Retention Scheme statistics: July 2021’ July 2021. ↩
-
DHSC/CO, ‘COVID-19 mental health and wellbeing recovery action plan’, March 2021. ↩
-
18% of small employers, compared to 92% of large employers, invest in OH. Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981, July 2021. ↩
-
See Annex A for Costs and Benefits: Overview and Methodology. ↩
-
ONS - A08: Labour market status of disabled people, July 2021. ↩
-
DWP/DHSC. ‘Health in the Workplace – Patterns of sickness absence, employer support and employment retention’ July 2019. ↩
-
The proportion of those staying in work following their long-term sickness absence (or longest LTSA) decreases as the duration of long-term sickness absence increases. Those whose LTSA spell lasts for 1 year or more are 8 times more likely to leave work following their LTSA than those with a 4-week duration. DWP/DHSC. ‘Health in the Workplace – Patterns of sickness absence, employer support and employment retention’ July 2019. ↩
-
DWP/DHSC. ‘Health in the Workplace – Patterns of sickness absence, employer support and employment retention’ July 2019. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
See Annex B DWP/DHSC. ‘Interim summary of findings: Discrete choice experiment exploring impact of incentives on SME uptake of health and wellbeing support schemes’ July 2021. ↩
-
ONS - A08: Labour market status of disabled people, July 2021. ↩
-
ONS. ‘Coronavirus and the social impacts on disabled people in Great Britain: September 2020’ November 2020. ↩
-
Citizens Advice. ‘An unequal crisis: why workers need better enforcement of their rights’ August 2020. ↩
-
DWP/DHSC, ‘Improving lives: the future of work, health and disability’ November 2017. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
See Annex B DWP/DHSC. ‘Interim summary of findings: Discrete choice experiment exploring impact of incentives on SME uptake of health and wellbeing support schemes’ July 2021. ↩
-
See Annex B DWP/DHSC. ‘Interim summary of findings: Discrete choice experiment exploring impact of incentives on SME uptake of health and wellbeing support schemes’ July 2021. ↩
-
Bajorek Z and others. ‘Working from Home under COVID-19 lockdown: Transitions and Tensions’ Economic & Social Research Council (ESRC) January 2021. ↩
-
DWP/DHSC. ‘Health in the Workplace – Patterns of sickness absence, employer support and employment retention’ July 2019. ↩
-
Dekkers-Sánchez P.M and others. ‘Factors associated with long-term sick leave in sick-listed employees: a systematic review’ Occupational and environmental medicine, Volume 65, Issue 3, pages 153 to 157 April 2008. ↩
-
Daniels K and others. ‘Sustainable Return to Work: A Systematic Review Focusing on Personal and Social Factors’ Journal of occupational rehabilitation, Volume 29, Issue 4, pages 679 to 700 February 2019. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
DWP. ‘Understanding the journeys from work to Employment and Support Allowance (ESA)’ June 2015. ↩
-
AXA Asia/Columbia University WHO Centre for Global Mental Health. ‘Supporting Mental Health of Employees During and Beyond COVID-19’ June 2020. ↩
-
Bajorek Z and others. ‘Working from Home under COVID-19 lockdown: Transitions and Tensions’ Economic & Social Research Council January 2021. ↩
-
CIPD. ‘Absence measurement and management’ April 2021. ↩
-
Other SSP eligibility criteria applies. ↩
-
Viikari-Juntura E and others. ‘Return to work after early part-time sick leave due to musculoskeletal disorders: a randomised controlled trial’ Scandinavian Journal of Work, Environment and Health, Volume 38, Issue 2, pages 134 to 143 November 2012. ↩
-
Simen M and others. ‘The case for presenteeism – Evidence from Norway’s sickness insurance program’ Journal of Public Economics, Volume 96, Issue 11-12, pages 959 to 972 December 2012. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
biopsychosocial approaches systematically consider biological, psychological, and social factors alongside their complex interactions in understanding health, illness, and health care delivery. ↩
-
Ballard J. ‘SURVEY: Occupational health and the COVID-19 pandemic, part 1 - An exclusive survey for Occupational Health [at Work]’ Volume 17, Issue 1 June/July 2020. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
DWP/DHSC. ‘Health in the Workplace – Patterns of sickness absence, employer support and employment retention’ July 2019. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
Fullick S and others. ‘Employers’ motivations and practices: A study of the use of occupational health services’ /DWP/DHSC report number 979 April 2019. ↩
-
Fullick S and others. ‘Employers’ motivations and practices: A study of the use of occupational health services’ DWP/DHSC report number 979 April 2019. ↩
-
See Annex B DWP/DHSC. ‘Interim summary of findings: Discrete choice experiment exploring impact of incentives on SME uptake of health and wellbeing support schemes’ July 2021. ↩
-
Mintel. ‘Occupational Health: Inc Impact of COVID-19 – UK – May 2020’ May 2020. ↩
-
Ballard J. ‘SURVEY: Occupational health and the COVID-19 pandemic, part 1 - An exclusive survey for Occupational Health [at Work]’ Volume 17, Issue 1 June/July 2020. ↩
-
‘DWP COVID-19 Employer Pulse Survey Interim summary report’ DWP ad hoc report number 78 July 2021. ↩
-
Bank of England. ‘Impact of Covid-19 on UK businesses – evidence from the Decision Maker Panel in 2020 Q4’ December 2020. ↩
-
Tindle A and others. ‘Understanding the provision of occupational health and work-related musculoskeletal services’ DWP/DHSC report number 985 May 2020. ↩
-
99% of OH providers used some form of training, development or accreditation system, and 96% of providers agreed that “the training, development and/or accreditation systems were effective in ensuring quality of service.”. Tindle A and others. ‘Understanding the provision of occupational health and work-related musculoskeletal services’ DWP/DHSC report number 985 May 2020. ↩
-
3% of all employers, and 23% of large employers, cite the reason for not providing OH services as lack of knowledge about what services to buy and who to buy from. Tu T and others. ‘Sickness absence and health in the workplace: Understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
See Annex B DWP/DHSC. ‘Interim summary of findings: Discrete choice experiment exploring impact of incentives on SME uptake of health and wellbeing support schemes’ July 2021: found that providing supplementary advice to SMEs in the form of a needs assessment and signposting to appropriate health and wellbeing schemes could increase take-up amongst SMEs. ↩
-
SEQOHS conducted a survey of their members to answer the consultation. This is in response to Q.46, ‘As a provider, what indicators of quality could help improve the standard of services in the OH market?’. ↩
-
Tindle A and others. ‘Innovation and knowledge development amongst providers of occupational health’ DWP/DHSC report number 992 July 2021. ↩
-
Tindle A and others. ‘Innovation and knowledge development amongst providers of occupational health’ DWP/DHSC report number 992 July 2021. ↩
-
Tindle A and others. ‘Innovation and knowledge development amongst providers of occupational health’ DWP/DHSC report number 992 July 2021. ↩
-
Tindle A and others. ‘Innovation and knowledge development amongst providers of occupational health’ DWP/DHSC report number 992 July 2021. ↩
-
Tindle A and others. ‘Understanding the provision of occupational health and work-related musculoskeletal services’ DWP/DHSC report number 985 May 2020. ↩
-
54% of employers are aware of the NHS 111 Isolation Note. Of those, 92% of employers would accept this as evidence for sickness absence or self-isolation, demonstrating flexibility in accepting medical evidence for SSP purposes. ‘DWP COVID-19 Employer Pulse Survey Interim summary report’ DWP ad hoc report number 78 July 2021. ↩
-
DWP/DHSC, ‘Improving lives: the future of work, health and disability’ November 2017. ↩
-
For a more detailed justification of policy options, please refer to the “How we consulted” section in the main document. ↩
-
DWP/DHSC. ‘Work, Health and Disability Green Paper Data Pack’ October 2016. Black C and others. ‘Health at work – an independent review of sickness absence’ DWP November 2011 ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021 ↩
-
Oxford Economics. ‘The cost of Brain Drain: Understanding the financial impact of staff turnover’ February 2014 ↩
-
Oxford Economics. The Cost of Brain Drain: Understanding the financial impact of staff turnover February 2014 ↩
-
The study aims to quantify the costs of labour turnover amongst workers earning above £25,000 per year in 5 key economic sectors (Retail, IT and Technology, Legal, Accounting, and Media and Advertising). ↩
-
The median is similar to the arithmetic mean for the values available - the average estimate is not sensitive to this choice. ↩
-
ONS – Earnings and hours worked, occupation by four digit SOC: ASHE table 14.1a, 2019 revised ↩
-
Oxford Economics. The cost of Brain Drain: Understanding the financial impact of staff turnover February 2014 ↩
-
ONS – Earnings and hours worked, occupation by four digit SOC: ASHE table 14.1a, 2019 revised ↩
-
Wage rates have been uprated to account for non-wage labour costs, in line with corresponding ONS data on labour costs: ‘Index of labour Costs per Hour, UK: October to December 2019’, March 2020 ↩
-
Individual A is employed by a company and individual B is a potential replacement. It is assumed that if individual A is kept in work, there is no change to individual B. This model is quantifying the benefit to keeping A in work, not the benefit to B getting into work in the event that A falls out of work. ↩
-
One in 5 employers offered OH services to their employees and this was more common amongst large (92%) than medium (49%) or small employers (18%). Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021 ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981July 2021 ↩
-
Only 5% of small employers used a HR team whereas 1 in 5 (20%) large employers used a HR team. Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981July 2021 ↩
-
Disabled employees working for small workplaces were over 1.5 times more likely to fall out of work compared to disabled employees working for large workplaces. DWP/DHSC. ‘Health in the Workplace – Patterns of sickness absence, employer support and employment retention’ July 2019. ↩
-
Bartley M. ‘Unemployment and ill health: understanding the relationship’ Journal of Epidemiology and Community Health, Volume 48, Issue 4, pages 333 to 337, August 1994. Davies S C. ‘Annual Report of the Chief Medical Officer 2013, Public Mental Health Priorities: Investing in the Evidence’ Department of Health September 2014. Lelliott P and others. ‘Mental Health and Work’ Royal College of Psychiatrists/Health Work Wellbeing March 2008. Burton A K and others. ‘Is work good for your health and well-being?’ TSO 2006. ↩
-
Public Health England. ‘Movement into employment: return on investment tool’ October 2017 ↩
-
QALYs are used in health-related appraisal. It is a single measure including two dimensions; length of life and health related quality of life ↩
-
Public Health England. ‘Movement into employment: return on investment tool’ October 2017 ↩
-
SF-36 is a validated 36-item Short Form questionnaire which measures quality of life across a set of eight domains, encompassing mental, physical and general wellbeing metrics. ↩
-
The methodology used to derive this range is implicitly assuming correlation between the eight SF-36 domains. ↩
-
Cullen K and others. ‘Workplace-based return-to-work interventions: a systematic review of the quantitative literature’ Journal of occupational rehabilitation, Volume 15, Issue 4, pages 607 to 631 December 2005 ↩
-
Dekkers-Sánchez P M and others. ‘What promotes sustained return to work of employees on long-term sick leave? Perspectives of vocational rehabilitation professionals’ Scandinavian journal of work, environment & health, Volume 37, Issue 6, pages 481 to 493 November 2011 ↩
-
We learned from employer and employee insight group responses to the consultation that SMEs in particular feel afraid to act in case they do the wrong thing. ↩
-
25% of small, 72% of medium and 69% of large employers have a sickness absence management policy in place. Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021 ↩
-
Small employers reported a lack of time or staff resources (64%) and a lack of capital to invest in support (51%). Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021 ↩
-
Only 5% of small employers used a HR team whereas 1 in 5 (20%) large employers used a HR team. Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021 ↩
-
ONS – Earnings and hours worked, age group by occupation by two digit SOC: ASHE table 20.5a, 2019. ↩
-
ONS. ‘Index of labour Costs per Hour, UK: October to December 2019’, March 2020 ↩
-
BEIS. ‘Business population estimates for the UK and regions 2020: statistical release’ October 2020 ↩
-
BEIS. ‘Business population estimates for the UK and regions 2020: statistical release’ October 2020 ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021 ↩
-
DWP/DHSC. ‘Health in the Workplace – Patterns of sickness absence, employer support and employment retention’ July 2019. ↩
-
ONS - Earnings and hours worked, age group by occupation by two digit SOC: ASHE table 20.5a, 2019. ↩
-
ONS. ‘Index of labour Costs per Hour, UK: October to December 2019’, March 2020. ↩
-
One in 5 employers offered OH services to their employees and this was more common amongst large (92%) than medium (49%) or small employers (18%). Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
ONS. ‘Sickness absence in the UK labour market 2020’ March 2021. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
-
Tu T and others. ‘Sickness absence and health in the workplace: understanding employer behaviour and practice’ DWP/DHSC report number 981 July 2021. ↩
